Eyeing New Therapies for Metastatic Uveal Melanoma
Moffitt Cancer Center is leading a five-year research project taking a closer look at the mechanisms behind uveal melanoma, a rare type of eye cancer, including why the disease often spreads to the liver and ways to treat it. The project is in collaboration with the Sylvester Comprehensive Cancer Center at the University of Miami and the University of Florida Health Cancer Center.
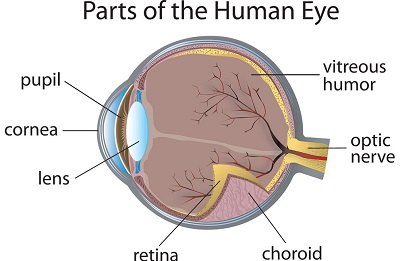
Uveal melanoma is rarer than melanomas of the skin. Approximately 7,000 people worldwide are diagnosed each year. It often goes undetected, as the most common place it develops is in tissue surrounding the back of the eye known as the choroid layer.
Like skin melanomas, uveal melanoma starts in melanocytes, the pigment cells that give color to the eyes. However, its cause is unknown, as it is not closely linked to UV light exposure. Those with a fair complexion, blue or green eyes, and fair or red hair tend to be more at risk for developing this type of cancer. But having been diagnosed with a skin melanoma does not necessarily increase your risk.
Understanding the Genetics
Dr. Keiran Smalley, director of Moffitt’s Donald A. Adam Melanoma and Skin Cancer Center of Excellence, has been working with Dr. Jonathan Licht, director of the University of Florida Health Caner Center, and Dr. J. William Harbour, associate director for basic science at Sylvester Comprehensive Cancer Center, since 2016 to better understand the mechanisms driving uveal melanoma. The team received two grants from the state of Florida to further their research, and their initial findings helped them receive a $3.95 million, five-year grant from the National Institutes of Health.

“Uveal melanoma is a highly aggressive disease. Even with treatment, nearly half of patients will develop metastatic disease, most commonly affecting the liver,” said Smalley. “Our team is studying two mutations that we believe play a role in disease progression and metastasis.”
The first mutation in the Gαq signaling pathway is seen in roughly 95% of all uveal melanoma cases. It allows for uveal melanocytes to rapidly multiply. In most instances, these cells go into growth arrest and the excess melanocytes become a mole. However, some of the Gαq-mutant cells can lay dormant. If these then acquire a mutation in the tumor suppressing BAP1 protein, it can allow for those mutated cells to awaken, multiply and spread to the liver. The researchers believe this mutation could be a factor in determining why uveal melanoma so often metastasizes to the liver.
“These two mutations, Gαq and BAP1, are rarely seen together in other cancers. Our work aims to understand why this happens in uveal melanoma and how these mutations cooperate allowing the uveal melanoma cells to colonize the liver,” said Smalley.
Developing New Therapies
Early-stage uveal melanoma can be treated with lasers, radiation or by removing the eye. Despite successful treatment of the primary tumor, nearly half of patients will develop metastatic disease several years later. Current immunotherapy drugs showing progress against skin melanomas are far less effective for metastatic uveal melanoma.
The research team is investigating two epigenetic proteins, HDAC1 and HDAC4, that are overexpressed when BAP1 is mutated. They believe HDAC inhibitors can be used to stop malignant cells from growing and induce an immune response, killing the cancer cells.
“We expect this work to lead to a future clinical trial and hopefully better outcomes for uveal melanoma patients,” said Smalley.



