What is a Bone Marrow Transplant (BMT)?
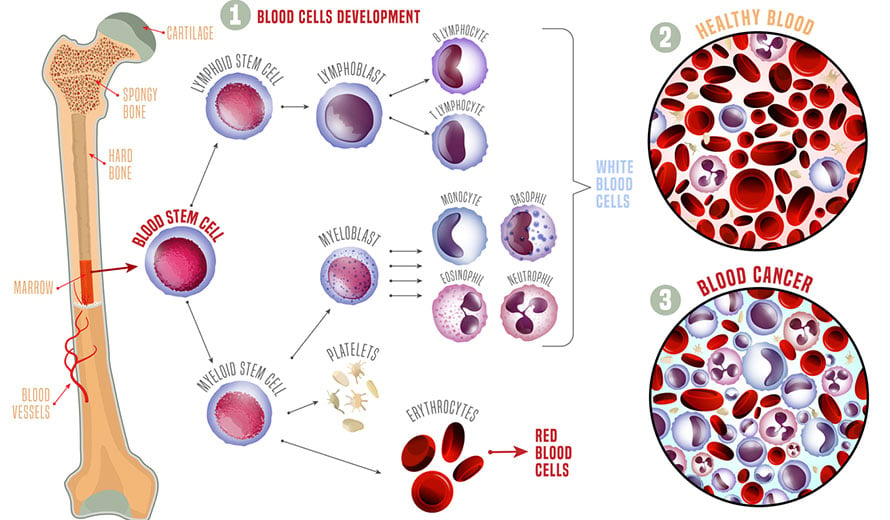
A spongy tissue found in the center (medullary cavities) of bones, bone marrow produces blood stem cells that mature into red blood cells, white blood cells and platelets. As such, healthy bone marrow is essential to sustain life.
What is a bone marrow transplant?
Sometimes, diseases such as cancer can affect the bone marrow, preventing it from making these essential cells. In other cases, a cancer patient’s chemotherapy or radiation treatment may damage or destroy healthy bone marrow so that it no longer generates the blood cells the patient needs. In these instances, a bone marrow transplant (BMT) may be necessary.
How does a bone marrow transplant work?
A bone marrow transplant takes healthy blood-forming cells from a donor and infuses those cells into the patient’s bloodstream, where the cells may begin to grow and produce healthy red blood cells, white blood cells and platelets. The healthy cells for transplantation have been previously collected from the patient or a donor that has been screened and determined to be an appropriate match. When it’s time for the transplant, the patient receives the donated cells through an intravenous (IV) catheter, or tube.
Many prospective patients understandably wonder: Does a bone marrow transplant hurt? In most cases, though, there is no bone marrow transplant pain. The patient remains awake throughout the entire process, and it is not uncomfortable. In fact, the bone marrow transplant procedure is very similar to receiving blood or medication through an intravenous (IV) catheter or tube. For many patients, the treatment is a significant step that holds tremendous meaning. Some continue to remember and celebrate the day long into the future, much like a second birthday.
How do you prepare for a bone marrow transplant?
Several steps must be taken to prepare the patient for a bone marrow transplant. First, a series of tests must be administered to determine if the patient is healthy enough to undergo the transplant, which is a lengthy process that can be both physically and emotionally taxing. Next, a catheter (central line) may be inserted into a vein in the patient’s chest, where it will remain for the duration of the treatment.
After these initial steps are completed, the patient will begin conditioning therapy. Typically, this process involves a course of high-dose chemotherapy and sometimes radiation therapy to prepare the patient’s body for the transplant, suppress his or her immune system and destroy any residual cancer cells. Transplant conditioning can take several days, although the duration and dosages can vary depending on factors unique to the patient. Once the conditioning process is complete, the patient will be ready to receive the stem cell transplant.

"Don't give up. Fight through.
You can do it."
-Nick, Stem Cell Transplant Survivor
Schedule an AppointmentWhat are the types of bone marrow transplants?
There are three types of blood and bone marrow transplants: autologous, in which the stem cells are taken from the patient’s own blood; allogeneic, in which the stem cells are collected from a donor; and syngeneic, in which the stem cells are obtained from an identical twin.
Autologous transplants
An autologous stem cell transplant may be used to treat several types of blood cancer. In an autologous transplant, the bone marrow transplant donor is also the recipient. The stem cells, which are harvested from the patient’s bone marrow and/or bloodstream, are typically collected when the cancer is in remission or has stabilized. Before the transplant is scheduled to take place, the patient begins conditioning therapy. This high-dose chemotherapy is effective at killing cancer cells, but also will destroy the patient’s bone marrow. Because of this, the stored stem cells of the patient are then used to restore the injured bone marrow. Specifically, once the conditioning therapy is complete, the stem cells are reintroduced to the patient's bloodstream via the central line. These stem cells then move into the patient’s bones and grow new bone marrow to replace the bone marrow that was eliminated by the chemotherapy.
Allogeneic (AN) transplants
 Sometimes recommended for patients with leukemia, an AN bone marrow transplant uses bone marrow from a donor who is a genetic match to the patient. Oftentimes, a sibling is a good candidate for an allogeneic stem cell transplant. Similarly, a syngeneic transplant involves collecting healthy stem cells from a donor who is the patient’s identical twin.
Sometimes recommended for patients with leukemia, an AN bone marrow transplant uses bone marrow from a donor who is a genetic match to the patient. Oftentimes, a sibling is a good candidate for an allogeneic stem cell transplant. Similarly, a syngeneic transplant involves collecting healthy stem cells from a donor who is the patient’s identical twin.
Extensive DNA testing on any potential donor is required to ensure that the donor’s stem cells and white blood cells are an appropriate match for the patient. It is more likely that the human leukocyte antigen (HLA) will match if the donor is the patient’s sibling rather than an unrelated donor. However, if the transplant recipient does not have a sibling or is not a match with his or her siblings, stem cells from an unrelated donor may be utilized. How is a bone marrow transplant done? To prepare for the transplant, the patient will first receive conditioning therapy which usually involves high doses of chemotherapy and radiation therapy. Then, the donor’s stem cells and white blood cells are infused into one of the patient’s veins, similar to a blood transfusion.
Even if the patient and donor are not a perfect match, a bone marrow stem cell transplant may still be the best treatment option for the patient.
Syngeneic transplants
A BMT for which the donor is the patient’s identical twin is the least complicated bone marrow transplantation because there’s no risk of rejection, graft-versus-host disease or tumor in the marrow.
What does a bone marrow transplant treat?
A bone marrow transplant is a common form of treatment for several conditions. For instance, a stem cell transplant may be beneficial to a patient who has:
- Acute leukemia
- Chronic leukemia
- Hodgkin lymphoma
- Non-Hodgkin lymphoma
- Lupus
- Multiple myeloma
- Multiple sclerosis
- Myelodysplastic syndromes
- Myelofibrosis
- Myeloproliferative neoplasms
- Paroxysmal nocturnal hemoglobinuria (PNH)
- Primary amyloidosis
- Severe anaplastic anemia (SAA)
- Testicular cancer
- Waldenstrom’s macroglobulinemia
- Essential thrombocytosis (ET)
- Ewing’s sarcoma
While a blood and bone marrow transplant may be used to treat these conditions, it is important to note that the procedure is not right for everyone. To determine if a transplant is the best option for a patient, a multispecialty team will thoroughly review the specifics of the patient’s case.
What’s involved in bone marrow donation?
For patients who don’t have their own healthy cells to donate for their BMT, doctors look for a donor whose tissue type matches the patient’s for a certain protein, or marker, known as human leukocyte antigen (HLA). The body’s immune system uses HLA markers to distinguish between cells that ought to be present in the blood and those that shouldn’t. Therefore, incompatible HLAs can trigger an immune response, and the patient faces a higher risk of rejecting the transplanted cells.
Blood marrow donors are in high demand, as only about 30% of people who need a donor can find an HLA-matched family member to step in. Potential donors can register with the National Marrow Donor Program (NMDP) and either receive a mail-in kit or visit a donor center to provide a cheek swab or blood sample for analysis. Once the sample is analyzed, the volunteer donor’s HLA type is recorded in the NMDP database. Then, if an HLA match with a prospective BMT patient is identified, the NMDP contacts the prospective donor to confirm the match and provide information about the donation procedure.
If you’re a donor who’s matched to a patient that needs a transplant, you’ll meet with a representative of Be The Match® to complete a health questionnaire and go over the details of the donation procedure. If you agree to move forward with your donation, you’ll also undergo a physical exam and give blood samples.
A blood marrow donation requires surgery in a hospital operating room, during which you’ll be given anesthesia and doctors will use needles to withdraw liquid marrow from your pelvic bone. You may go home late the same day or be kept in the hospital overnight for observation. You may experience side effects; hip or back pain and fatigue are the most common. Most donors return to work or school within seven days. Donors do not incur medical costs.
Moffitt Cancer Center's approach to blood and bone marrow transplants
At Moffitt Cancer Center, we understand that a blood and bone marrow transplant can seem intimidating to a patient. A top concern, among others: Is a bone marrow transplant painful? Again, it is not. However, the procedure does require a significant commitment on the part of both the patient and his or her caregivers. Moffit’s compassionate team is available to provide comprehensive support to our transplant recipients every step of the way. For instance, we can help our patients manage any bone marrow transplant side effects, such as nausea, vomiting, diarrhea, anemia and fatigue, as well as any bone marrow transplant complications, such as infection and graft-versus-host disease (GVHD).
Another common question we hear from prospective patients is whether a bone marrow transplant changes DNA. To answer that question in the right context, it is important to note that the goal of a bone marrow transplant is to replace weak blood with healthy blood—and, in so doing, to save the recipient’s life. If the healthy blood comes from a donor, along with it may come some of the donor’s DNA. However, this effect is harmless, and it will not change the recipient’s brain or personality in any way.
Some patients also wonder about the bone marrow transplant procedure for the donor. Many mistakenly believe that donating blood stem cells is painful, but it is generally not, although some donors do experience mild to moderate discomfort during the recovery process, such as back pain, fatigue, headache or bruising. Typically, any discomfort resolves within a few days or weeks, and the vast majority of donors say it is worth it to help save a life—and they would do it again in a heartbeat.
To determine whether a patient is a good candidate for a bone marrow transplant, Moffitt’s transplant team will evaluate the patient’s age, individual care needs and medical history. During this process, we will also consider the various transplant techniques to determine which would be most beneficial to the patient.

If the patient requires an allogeneic transplant but does not have a sibling who can donate, Moffitt can search for a suitable volunteer donor through the National Marrow Donor Program. Currently, more than half of our allogeneic transplants are arranged with a volunteer donor, although an HLA match must still be obtained. Moffitt will also screen potential donors to ensure they can tolerate a stem cell harvest and that they do not have any active infections or other complications that might negatively impact their ability to donate.
When a patient is cleared for a blood or bone marrow transplant procedure, Moffitt’s experienced physicians, nurses, lab technicians, transplant coordinators, dietitians and other medical professionals work together to provide individualized care at every phase of the transplant process. This approach helps us achieve the best possible outcome while enhancing the patient’s quality of life.
Medically reviewed by Hany Elmariah, MD, MS
If you have questions about our approach to blood and bone marrow transplantation or the difference between a stem cell transplant vs. a bone marrow transplant, you can request an appointment with a specialist at Moffitt Cancer Center. To do so, call 1-888-663-3488 or complete a new patient registration form online. Your cancer diagnosis is our top priority, and we will make sure you can speak with a cancer expert as soon as possible.

