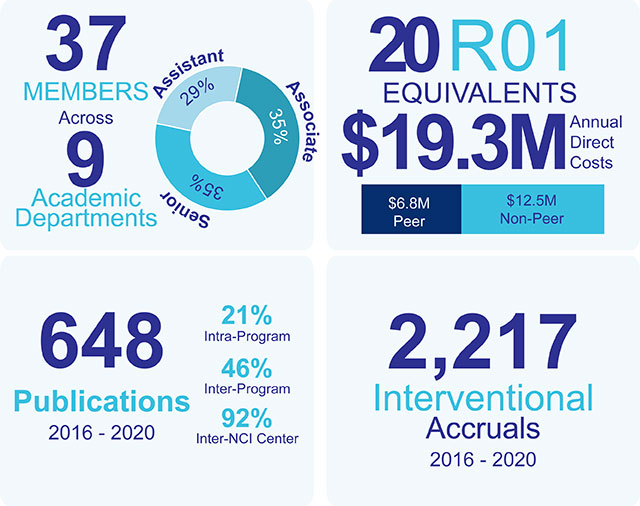
Immuno-Oncology Program Scientific Highlights
Examples of high impact IO research and clinical trials that foster meeting the goal of implementing superior anti-cancer immunotherapies by aim are as follows:
Aim 1:
Addressing major gaps of knowledge in the field, Dr. Conejo-Garcia, in collaboration with Drs. Rodriguez (IO) and Luca (MM), published a seminal study in Science, 20201, that revealed a novel checkpoint inhibitory pathway mediated by CD277+ butyrophilin family proteins in the microenvironment of human ovarian cancer. Importantly, in its spontaneous conformation at tumor beds, CD277+ butyrophilins (BTN3A1-3) impair TCR activation upon antigen recognition, by preventing segregation of CD45 from the immune synapse. Notably, anti-CD277 antibodies generated in collaboration with industry elicit conformational changes that abrogate their inhibitory activity on αβ T cells, and that transform BTN3A into immunostimulatory molecules for γδ T cells (Fig. 3). This has exciting implications for planned clinical trials in patients resistant to PD-1 or CTLA4 inhibitors.
IO Members have also made seminal contributions to understanding the role of ER stress in cancer-associated immune cells. First, mechanistic studies led by Dr. Rodriguez, published in Immunity, 20203 in collaboration with Dr. Conejo-Garcia, revealed that PERK, a driver of the UPR, governs the immunosuppressive function of intratumoral MDSCs. Specifically, PERK signaling is increased in tumor-MDSCs, and its deletion transformed MDSCs into activators of tumor-reactive T cells. Thus, it is feasible to transform tumor-associated myeloid cells from an immunosuppressive to an immunostimulatory phenotype, an approach that is potentially more effective than merely depleting MDSCs or macrophages in cancer patients.
Breast cancer is the leading cause of cancer among women in Moffitt’s catchment area, with disparities in mortality for Black women. In a collaborative study published in Cancer Cell, 20188, Drs. Ruffell and Soliman demonstrated that TIM-3 expression in intratumoral CD103+ dendritic cells can be targeted to boost anti-tumor immunity. Specifically, treatment with anti-TIM-3 antibody improved responses to paclitaxel in models of triple-negative and luminal B disease, with no evidence of toxicity and in a CD8+ T cell dependent manner. These studies establish roles of TIM-3 in dendritic cells (in addition to those in lymphocytes) and help explain emerging results of ongoing clinical trials blocking TIM-3. This work is especially relevant to our Black and Hispanic communities, who are more likely to be diagnosed with triple negative disease (Cancer, 20199).
Aim 2:
The work of thoracic oncologists in IO continued driving changes in clinical practice for lung cancer, which is observed at higher rates in our catchment area than in the US or Florida. A team led by Dr. Antonia* conducted a multicenter study involving >700 patients, published in the N Engl J Med, 201712, which demonstrated that the PD-L1 inhibitor durvalumab significantly prolongs overall survival in patients with unresectable, stage III Non-Small Cell Lung Cancer (NSCLC), This is important as other potential treatments for this set of patients (e.g., vaccines) have performed poorly. In follow-up studies published inLancet Oncol, 201913, the same team showed the clinical benefit of durvalumab was manifest without compromising patient-reported outcomes. These studies led to implementation of checkpoint inhibitors in lung cancer patients. Additional important studies reported in Lancet Oncology established that first-line nivolumab plus ipilimumab had a tolerable safety profile and a high and durable response rate (Lancet Oncol, 201715).
Moffitt has one of the highest volume hematopoietic marrow transplant programs in the country, with >430 patients transplanted annually. Drs. Pidala, Betts*, and Anasetti*, in collaboration with N. Lawrence (MM) and H. Lawrence (MM), have developed novel interventions for preventing GVHD, which remains the main cause of non-relapse mortality after allogeneic hematopoietic cell transplantation. In a publication in Sci Transl Med, 201717, this team showed that concurrent blockade of Aurora A and JAK2 kinases synergizes to prevent GVHD while maintaining antitumor responses by cytotoxic T lymphocytes (CTL). Mechanistically, Aurora A/JAK2 inhibition was shown to drive differentiation of inducible regulatory T cells (iTregs) that are hyperfunctional, CD39High and efficiently scavenge ATP. Further, increased iTreg potency was due to Aurora A blockade, whereas JAK2 inhibition suppresses T helper 17 (TH17) differentiation.
Drs. Kim and Mulé, in collaboration with Dr. Berglund (MM), investigated the methylation status of key immune synapse genes across multiple human malignancies. In their study published in the J Clin Invest, 202021, the authors showed co-stimulatory genes are disproportionately hyper-methylated, while immune checkpoint genes are hypomethylated. Importantly, these signatures are negatively associated with the recruitment of functional T-cell to the tumor and with survival. The same team, in collaboration with Drs. Conejo-Garcia and Creelan, reported in Cell Metab, 202022 that the HDAC SIRT2 acts as a metabolic checkpoint inhibitor in tumor-infiltrating lymphocytes (Fig. 4). Strikingly, these studies revealed that mechanistically SIRT2 dampens the metabolism of effector T cells by directly deacetylating enzymes that orchestrate glycolysis, the TCA cycle, glutaminolysis and fatty acid oxidation. Accordingly, SIRT2 inhibition reprograms T cell metabolism to confer superior anti-tumor immunity.
Aim 3
Moffitt has one of the largest CAR T cell therapy clinical programs in the nation. Dr. Locke was co-lead Principal Investigator of the ZUMA-1 worldwide study in patients with refractory large B-cell lymphoma. These practice changing results, published in the N Engl J Med, 201726, demonstrated that the CD19-directed CAR T cell therapy, axicabtagene ciloleucel (axi-cel), has a high complete response rate in chemotherapy refractory patients (Fig. 5), with an acceptable safety profile that included myelosuppression, cytokine release syndrome, and neurologic events. ZUMA-1 was a landmark study as it showed that gene-engineered T-cells could be rapidly generated and safely administered across multiple institutions, which led to FDA approval. Indeed, ASCO selected CAR T cell therapy as its “2018 Advance of The Year”, including a citation of ZUMA-1.
Moffitt remains one of the five Centers that is FDA approved for the production of TILs. Iovance Biotherapeutics established its headquarters in the vicinity of Moffitt to collaborate with IO Members on new clinical trials. Leveraging this long-term collaboration, Drs. Creelan, Pilon-Thomas, Kim, Antonia* and Conejo-Garcia collaborated with Drs. Haura (MM) and Teer (CBE) on a clinical trial targeting NSCLC that is co-supported by Stand Up to Cancer. Importantly, in response to ex vivo expanded, adoptively transferred TIL that were collected before the start of checkpoint inhibitor therapy, objective partial responses, including 2 complete responses, have been observed in most NSCLC patients resistant to PD-1 inhibitors. These results were presented at the AACR Virtual Annual Meeting and were highlighted in Cancer Discov, 202032.
Melanoma is a priority cancer in Moffitt’s catchment area, with rates that are higher than those in the state and much higher than those in the nation. To tackle this disease a multi-disciplinary team that includes Drs. Sarnaik, Sondak, Pilon-Thomas and Mulé, are investigating new treatments for this malignancy leveraging the Donald A. Adam Melanoma & Skin Cancer Center of Excellence. Recent advances of a pivotal Moffitt-led multicenter study combining TIL transfer with CTLA4 blockade, published in Front Oncol, 201833, and presented by Dr. Sarnaik at the 2020 ASCO Annual Meeting, have demonstrated a 36% response rate to TIL among patients with unresectable, immunotherapy-resistant cutaneous melanoma. These responses exceed 12 months in most patients and, most importantly these findings are expected to lead to FDA to approval for widespread use of TIL transfer therapies.
Immuno-Oncology
