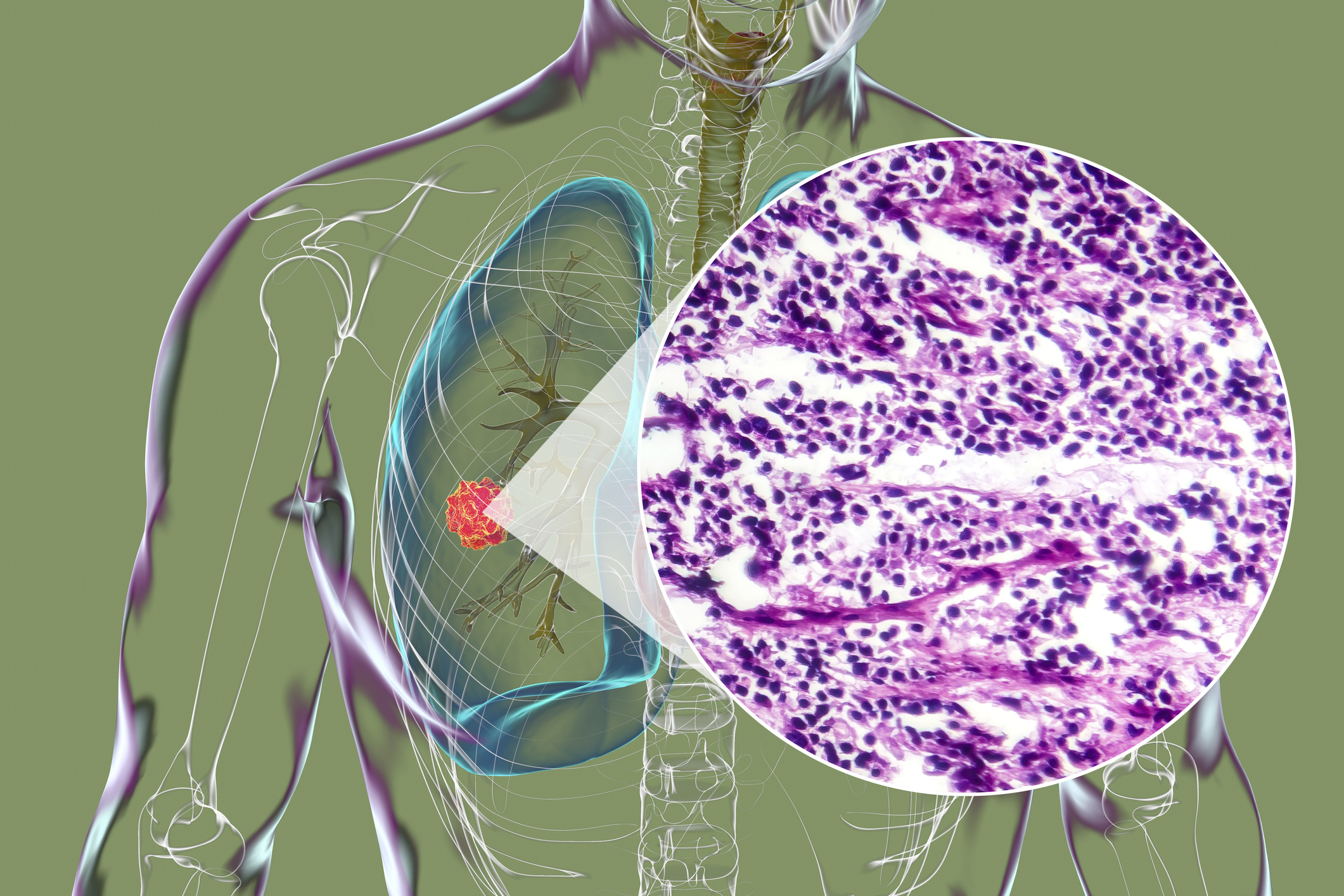
Immunotherapy for Lung Cancer
The immune system is programmed to identify and destroy any foreign or pathogenic cells that it doesn’t recognize, so cancer cells should be recognized and targeted because they are not normally found in the body. However, cancer develops gradually as healthy cells undergo a series of subtle DNA mutations and acquire the ability to evade the immune system. Immunotherapy is one of the most promising new treatments for lung cancer, since it helps the body’s immune system to locate and destroy cancerous cells.
How does immunotherapy treat lung cancer?
Different immunotherapy drugs work in different ways. Some trigger the body’s natural immune system response, while others kick-start cell destruction in a manner that differs from the body’s usual processes. Other immunotherapy drugs can override the immune system’s “off switch” that otherwise prevents it from attacking cancerous cells. In these ways, immunotherapies can specifically target cancerous cells that have abnormal growth patterns while leaving healthy cells unaffected.


Lung Cancer Outcomes More than Double the National Average
OutcomesTypes of immunotherapies for lung cancer
There are two main types of immunotherapies that are used to treat lung cancer: immune checkpoint inhibitors and T-cell therapies.
Checkpoint inhibitors
Immune checkpoints function as an on/off switch for the immune system, which normally prevents the immune system from destroying healthy cells. Proteins on the surface of immune cells called T cells match with partner proteins on other healthy cells, which turns off the immune response. Some tumor cells possess partner proteins that can trick the immune system into not attacking. Checkpoint inhibitors work by blocking the T cell proteins from binding with the proteins on the cancerous cells, which then signals the immune system to destroy the cancer.
There are many types of checkpoint inhibitor medications that may be used to treat lung cancer, including:
- Ipilimumab
- Bevacizumab
- Ramucirumab
- Nivolumab
- Pembrolizumab
- Atezolizumab
- Durvalumab
- Osimertinib
Some of these medications can also be used to treat other types of cancer. For example, ipilimumab is FDA-approved for the treatment of melanoma as well. To determine the medication that’s best for each patient’s unique needs, a team of medical oncologists, pathologists and other specialists will jointly discuss the patient’s diagnostic information and test results.
Adoptive T-cell therapies
A more aggressive type of immunotherapy is adoptive T-cell therapies, which include transgenic T-cell receptor (TCR) infusions and chimeric antigen receptor T-cell (CAR-T) infusions. These cellular immunotherapy treatments are only available for lung cancers through clinical trials. In these trials, the patient’s tumor is screened to see if it contains a specific protein. Then, the patient has a blood collection procedure to harvest their own T-cells. Next, the T-cells are genetically changed to express a special TCR or CAR which is unique for the tumor. Finally, the patients receive the engineered T-cell product, in a monitored setting. Examples of these trials at Moffitt include those being conducted with Adaptimmune and Kite pharmaceutical companies.
FDA Approvals
In May 2024 the FDA approved tarlatamab (Imdelltra, Amgen, Inc.) for extensive stage small cell lung cancer (ES-SCLC) with disease progression on or after platinum-based chemotherapy. Moffitt was the first health care provider in the United States to commercially treat a patient with tarlatamab and we are proud to be able to offer this kind of revolutionary therapy for our patients. The treatment is an engineered antibody that attaches to the surface of small cell lung cancer cells and immune cells, bringing the two together and using T-cells to kill the cancer.

What’s the difference between immunotherapy and other lung cancer treatment options?
Immunotherapy is different from other types of cancer treatments in that it specifically optimizes communication between the immune system and the cancer cells to help the body fight off cancer. Here is a brief summary of how other lung cancer treatment options work:
- Chemotherapy – Potent drugs are administered to destroy cancerous cells and prevent them from multiplying. While chemotherapy can be very effective for treating lung cancer, it can damage healthy cells too and cause significant side effects.
- Targeted therapy – Some lung cancer tumors can be treated with targeted therapy, which identifies and attacks cancer cells with specific molecular markers, preventing uncontrollable tumor growth. Since targeted therapies only attack cancer cells, there are fewer side effects associated with the treatment. However, these therapies only prevent tumor growth—they cannot destroy existing cancer cells.
- Radiation therapy – Advanced machines are used to deliver intense X-ray or proton beams that kill cancer cells. Radiation therapy can be delivered either internally or externally, and while it may harm some healthy cells in addition to cancer cells, healthy cells can generally repair themselves.
Who is a candidate for lung cancer immunotherapy?
Immunotherapy is typically used to treat patients with stage 3 or stage 4 lung cancer. It can be an effective treatment option for both small cell and non-small cell lung cancer. To determine if immunotherapy is a good treatment option—either alone or in conjunction with chemotherapy—a pathologist will conduct genomic testing of the lung cancer tumor, then check if there is an FDA-approved immunotherapy drug that matches the specific mutations present in the tumor. Since immunotherapy stimulates the immune system, it may not be a good treatment option for patients with autoimmune diseases.
Potential side effects of immunotherapy for lung cancer
While immunotherapy can cause fewer and less serious side effects than chemotherapy, patients may still experience:
- Fatigue
- Cough
- Nausea
- Itching
- Skin rash
- Loss of appetite
- Stomach pain
- Constipation or diarrhea
- Joint, muscle or bone pain
Some patients may also experience infusion reactions when receiving immunotherapy drugs, which present similar to allergic reactions with symptoms like:
- Fever
- Chills
- Flushed face
- Skin rash
- Itching
- Dizziness
- Trouble breathing
Immunotherapy drugs can also sometimes cause autoimmune reactions, where the immune system attacks healthy organs and cells. Left untreated, these side effects can be serious.
How effective is immunotherapy for treating lung cancer?
Immunotherapy is not an effective lung cancer treatment for everyone, since there are many different types of lung cancer and some patients respond more strongly than others to the treatment. However, it is a very promising treatment overall and can significantly extend life expectancy and improve quality of life for many patients.
Turn to Moffitt for cutting-edge lung cancer treatment
At Moffitt Cancer Center, we take a team approach to cancer treatment. A collaborative, multispecialty group of oncologists reviews each patient’s unique situation to recommend the most promising forms of treatment. Complex cases are presented during our weekly tumor board meetings. This allows us to create comprehensive, individualized treatment plans that incorporate the best surgical techniques, radiation therapy delivery methods, chemotherapy and immunotherapy medications as well as other novel treatments for lung cancer.
To learn more about immunotherapy for lung cancer, call 1-888-663-3488 or submit a new patient registration form online. You can make an appointment at Moffitt with or without a physician’s referral.
References
Immunotherapy for Lung Cancer
Lung Cancer Immunotherapy | Immune Checkpoint Inhibitors
Lung Cancer Immunotherapy