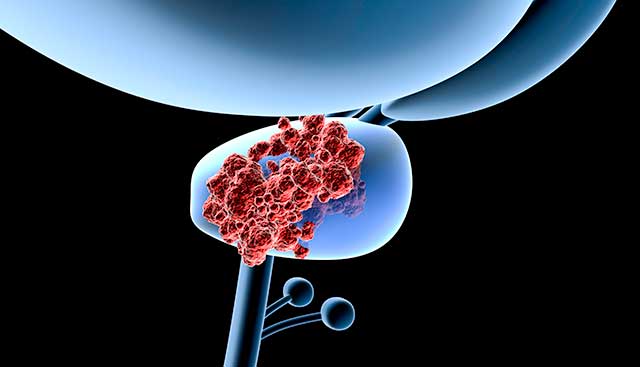
Promising CAR T-PSMA Clinical Trial in Patients with Metastatic Castration Resistant Prostate Cancer
Prostate cancer is one of the main causes of cancer-related death in men. Often, the diagnosis can be well managed, however, for patients who develop metastases and resistance to primary androgen deprivation therapy, the therapeutic options for metastatic castration resistant disease become limited.
Moffitt Cancer Center is opening a multi-center, open-label, Phase 1 clinical trial to identify the dose and regimen of CAR T-PSMA cells that can be safely administered intravenously following a lymphodepletion regimen to patients with metastatic castration resistant prostate cancer. The chimeric antigen receptor T-cell therapy (CAR T) is a genetically modified autologous T cells engineered to recognize prostate-specific membrane antigen (PSMA). The activated T cells then seek out and kill cancer cells.
The Moffitt Genitourinary Oncology program is focused on developing CAR-T cell therapeutics for prostate cancer patients adept at bypassing immune tolerance mechanisms. As opposed to hematologic malignancies, solid tumors tend to have more heterogeneity of disease and polyclonality. These factors make treating solid tumors with CAR-T more challenging due to a less immune attractive environment in the tumor itself. When considering target antigens, both prostate stem cell antigen (PSCA) and PSMA are seemingly high-potential target antigens for CAR-T cell clinical investigation for patients with prostate cancer.
As a genitourinary oncologist and part of this study assessing PSMA-directed therapy, Jingsong Zhang, MD, PhD represents the immunotherapy-specialized teams at Moffitt working on CAR-T cell therapy, and trials like this looking to expand CAR-T therapy so patients with solid tumors can be treated with these exciting therapies.
Eligibility criteria
The study can enroll up to 50 adult males who are 18 years and older.
Inclusion Criteria:
- Confirmed histologic diagnosis of prostate cancer and have mCRPC, with castrate levels of testosterone (<50 ng/mL)
- PSA measurable disease per Prostate Working Group 3 (PCWG3) criteria
- Prior therapies defined as at least 2 prior lines of systemic therapy for prostate cancer, including at least one second generation androgen receptor inhibitor and/or CYP17α inhibitor. At least one line of prior therapy must be in the mCRPC setting
- Estimated glomerular filtration rate ≥ 60 mL/min by Modification of Diet in Renal Disease criteria
- Alanine aminotransferase (ALT) and aspartate aminotransferase (AST) ≤ 2.5x the upper limit of normal (ULN); patients with hepatic metastases ALT and AST ≤ 3.0x ULN
- Serum total bilirubin < 1.5 mg/dL unless patient has known Gilbert's Syndrome, then serum bilirubin ≤3 mg/dL
- Serum albumin ≥ 3.0 g/dL
- Left ventricular ejection fraction (LVEF) ≥ 50%. LVEF assessment must have been performed within 8 weeks of enrollment
- Hemoglobin ≥ 8 g/dL
- Absolute neutrophil count ≥ 1000/μL
- Platelet count ≥ 75,000/μL
- Patients who have not undergone bilateral orchiectomy must be able to continue gonadotropin-releasing hormone (GnRH) therapy during the study
- Eastern Cooperative Oncology Group (ECOG) score of 0 or 1
- Toxicities from any previous therapy must have recovered to Grade 1 or baseline
- Patients of reproductive potential agree to use of approved highly effective contraceptive methods
Exclusion Criteria:
- Active invasive cancer, other than the proposed cancer included in the study, within 2 years prior to screening, unless treated with curative intent
- Current treatment with systemic corticosteroids (defined as a dose greater than the equivalent of prednisone 10 mg/day)
- Active autoimmune disease (including connective tissue disease, uveitis, sarcoidosis, inflammatory bowel disease or multiple sclerosis) or a history of severe autoimmune disease requiring prolonged immunosuppressive therapy (any immunosuppressive therapy within 6 weeks prior to screening visit)
- Current human immunodeficiency virus (HIV), hepatitis C virus, hepatitis B virus infections; Patients who are hepatitis B core antigen positive, hepatitis B surface antigen negative, should have a quantitative viral load measured; If viral load is undetectable, the patient will not be excluded if they are able to be treated with anti-viral medication for at least 7 days prior to lymphodepletion until at least 6 months after infusion with viral load and ALT monitoring
- Active or uncontrolled medical or psychological condition that would preclude participation
- Prior allogeneic stem cell transplant
- Active and untreated central nervous system malignancy
- History of severe infusion reaction to monoclonal antibodies or biological therapies, or to study product excipients that would preclude the patient safely receiving CART-PSMA-TGFβRDN cells
- History of being previously treated with a J591 antibody-based therapy
- Active or recent (within the past 6 months prior to apheresis) cardiovascular disease, defined as (1) New York Heart Association Class III or IV heart failure, (2) unstable angina, (3) a history of recent (within 6 months) myocardial infarction or sustained (> 30 second) ventricular tachyarrhythmias, or (4) cerebrovascular accident
- Have inadequate venous access for or contraindications for the apheresis procedure
- Must agree not to participate in a conception process or must agree to a highly effective method of contraception
If you are interested in learning more about clinical trials, our clinical trial navigators can discuss your options and recommend opportunities that may be suitable for you. Call 813-745-6100 or 1-800-679-0775 (toll-free) or submit a clinical trials inquiry form.
