What are Cancer Disparities?
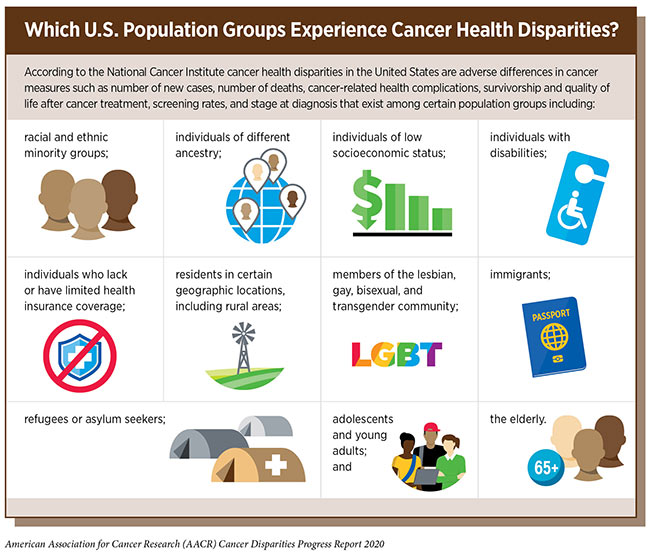
When it comes to health care, many minority populations are underrepresented and have difficulty accessing what they need to maintain healthy habits and lifestyles. The term “disparities” is used by those studying the phenomena, but what, exactly, does a disparity look like and how is it identified?
According to Dr. B. Lee Green, a senior member in Moffitt Cancer Center’s Department of Health Outcomes and Behavior, it all boils down to numbers.
“Disparity ‘is’ the numbers and the outcomes,” he said. “We can see there are differences in cancer morbidity and mortality among different populations and equity is the action. These numbers prompt us to discuss how we are going to address the disparity in front of us.”

Awareness months like Black History Month in February provide an opportunity to focus not only on the accomplishments of specific communities, but also on the challenges in equity that are present.
According to the American Association for Cancer Research Cancer Disparities Progress Report 2020, the African American population still shoulders a disproportionately high burden of overall cancer mortality compared with other racial and ethnic groups.
However, progress is being made. The disparity in the overall cancer death rate has narrowed from 33% higher for African Americans compared with whites in 1990 to 14% higher for African Americans in 2016, according to the report.
Even more encouraging, the disparity in the overall cancer death rate between African Americans and whites has been nearly eliminated among men younger than 50 and women 70 or older. The reductions occurred because the overall cancer death rate decreased more rapidly among African Americans than it did among whites during this period.
The report adds that racial and ethnic minority groups in the United States experience striking disparities in incidence and death rates for various types of cancer.
This is why identifying and studying disparities is so important to improve overall health outcomes and the quality of life for all populations, according to Green.
“Trust Has Been a Major Issue”
“When looking at specific communities and causes of disparities, we look at things like lack of understanding, cultural issues and access around health care,” Green said. “Trust has been a major issue within the Black community when it comes to health. There are people in our community who don’t trust doctors, the health care system or the government either because they had a bad experience or a family member had a bad experience. It’s difficult to pinpoint just one or two things that cause disparities and there are no one-size-fits-all solutions. But we must innovate, and we have to identify those disparities in order to address equity.”
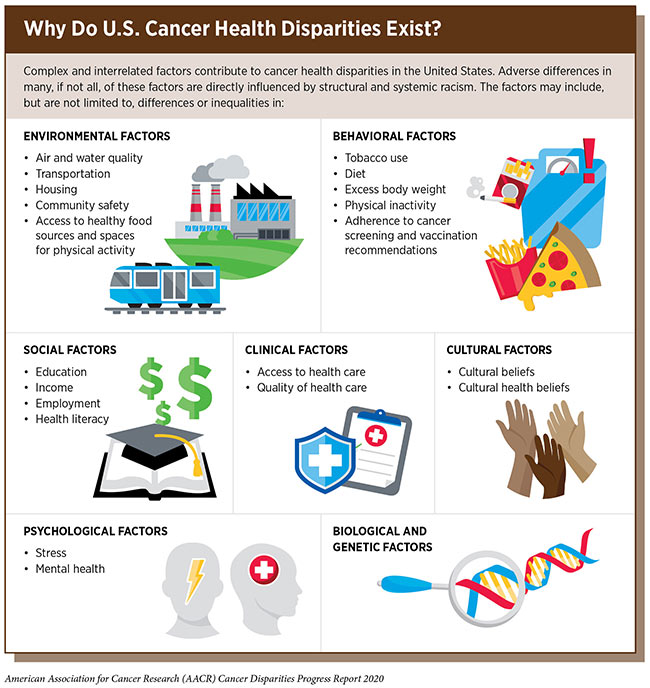
Disparities come in all types of forms. Where we live, where we play, where we work and where we get our health care are all factors, Green said. Social demographics are a key to identifying disparities, regardless of the ethnic community represented.
If someone is living in an impoverished location, for example, that will play into those challenges of finding adequate health care, nutrition and healthy activities. Locations can also influence diet, which is why food deserts are often a concern.
“When people aren’t located to a nearby market that has fresh fruits and vegetables, that can contribute to those disparities,” Green said. “And if home isn’t near a health care facility, that can play a role. We have to look at all of those things to factor in the higher risks certain populations may face, all because of their specific location or situation.”
Certain populations in the community suffer at a higher rate or at a different rate than the majority population. There is a significant difference between death rates and occurrence of disease in certain populations. Notably many of these disparities are in cancers that have screening strategies that help to detect cancer at an earlier, more treatable stage, and in some cases strategies to prevent cancer from developing.
“I will use prostate cancer as an example,” Green said. “Black men have a different death rate than white men and different occurrence of prostate cancer when you compare the two populations. The differences between Blacks and whites are significant.”
National guidelines recommend that men ages 55 to 69 who are at average risk of developing prostate cancer talk to a physician about the benefits and potential harms of screening before deciding if it is right for them. Some professional societies and organizations recommend that African American men begin this conversation at age 45 because the prostate cancer incidence rate is dramatically higher for them compared with men of any other race or ethnicity, which means that they are at increased risk.
However, even with that higher risk of prostate cancer, there is a large disparity in screening rates between Black men and their white counterparts. The AACR report shares that the disparity in prostate cancer screening between African American and white men exists even though African American men are more likely to report having been informed about prostate cancer screening than white men.
The AACR also shares that understanding the reasons for the low rates of prostate cancer screening among African American men informed about screening is vital if disparities in the burden of prostate cancer are to be eliminated.
Disparities Affect Men and Women
Black women are also impacted by disparities in cancer care. While the AACR reports that African American women have a higher cervical cancer incidence rate compared with white women, (7.4% to 6.3%, respectively), the reasons include social, clinical and environmental factors that affect socioeconomic status and access to quality cancer care, particularly timely guideline concordant cervical cancer screening coupled with follow-up for abnormal findings.
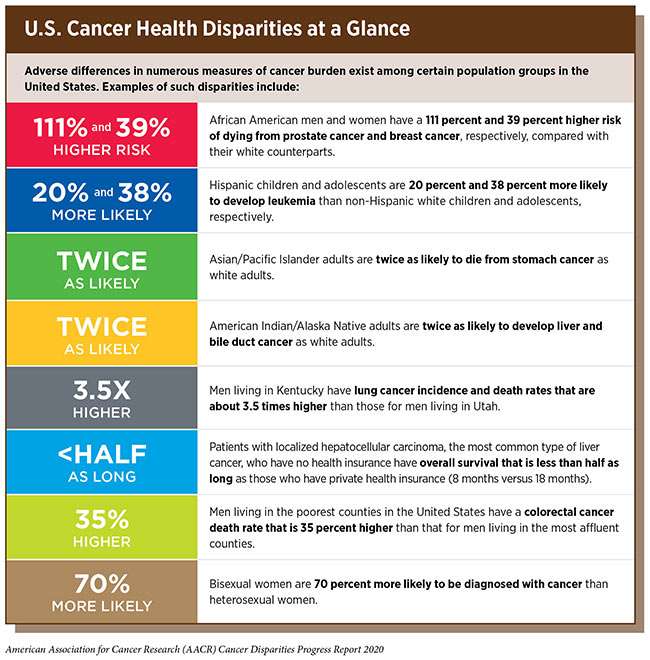
African American women are also more likely to be diagnosed with more advanced stage cervical cancer compared with white women, which may be because of differences in the approach to screening and timeliness of follow-up of abnormal results.
These are a few examples of why it is so important to study the root cause of cancer disparities to take the next step toward developing solutions, Green said.
Serving Close to Home
At Moffitt, teams of health care providers, researchers and other team members are focused on ongoing outreach to communities impacted by disparities. The cancer center’s Office of Community Outreach, Engagement & Equity (COEE) focuses on building partnerships with these communities by providing education, screening, opportunities for research and clinical trials in communities in the Tampa Bay area and throughout the state.
Dr. Susan Vadaparampil, associate center director of Community Outreach, Engagement & Equity, acknowledges that Moffitt has a responsibility to those the cancer center serves close to home.

“We need to bring the community to the table to tell us what their most pressing needs are and to help us understand how to shape solutions that fit our community,” Vadaparampil said. “That is our mandate as a National Cancer Institute-designated Comprehensive Cancer Center.”
While those studying disparities want to make sure specific populations are getting the education and information necessary to remain healthy, Green said it’s important to remember that cancer impacts everyone, regardless of their background.
“Cancer doesn’t care what your ethnicity is,” he said. “One of the things we don’t want to happen is people thinking cancers are targeting people based on whatever demographic they may be in.”
Every individual has a different circumstance, he said, and that’s why the notion of personalized medicine and care is so important.
“All of the factors that roll into you as a person may impact your risk for a cancer,” he said. “But not everyone has the same situation, and these different disparities all play into that.”
Improvements for All
Data collection and sharing of information with key stakeholders within and outside the institution is essential.
“To share that message effectively means partnering with organizations that have the most direct reach and trust for these communities, such as churches or community centers,” Vadaparampil said.
Reaching into communities directly and sharing data and knowledge about cancer rates, screening and overall health will only improve outcomes for everyone, Green said. And while comparisons are often made between ethnic and cultural lines, that doesn’t mean that one group is more important than another. Making the comparisons along racial lines is how we can see that disparities exist.
The white population tend to have better outcomes than other groups because those individuals typically have better access to health care and to health information. Green sees two sides of a coin with this data.
Getting everyone to at least the level of care and education that reflects the latest advances in our understanding of cancer prevention, early detection and treatment will help make significant progress in the disparities issue. However, it’s also important to continue improving treatment and education in the white community, as well, since that will only enhance health care for everyone.
“We should be thinking of the notion of a ‘rising tide lifts all boats,’ ” Green said. “Disparities work focuses on data of individual communities, yes. But the overall goal is to improve access to health care and resources for everyone, regardless of their background.”



