Many Cancers Affect Black Community More, Report Shows
Cancer impacts everyone, regardless of age, race, ethnicity, identity or sexual orientation, or location. But there are some cancers that seem to be more prominent in specific communities.
The Black and African American community, for example, faces specific disparities when it comes to different types of cancers. And the reasons behind those disparities can be many.
“For most cancers, African Americans seem to be doing worse,” said Dr. Brandon Blue, a malignant hematologist at Moffitt Cancer Center. “If you take the big cancers that are always talked about such as breast, for example, African Americans seem to have a worse prognosis. If you take prostate cancer, not only do we also have a worse prognosis, we typically get diagnosed at a younger age.”
The list of cancers that seems to disproportionately affect the Black community is “unfortunately long,” Blue admits.

According to the American Association for Cancer Research Cancer Disparities Progress Report 2020, the African American population still shoulders a disproportionately high burden of overall cancer mortality compared with other racial and ethnic groups.
African Americans are the second-largest racial and ethnic minority group in the United States, comprising about 13% of the population. For more than four decades, African Americans have had higher overall cancer incidence and death rates than all other racial and ethnic groups in the United States. An estimated 202,260 African Americans were diagnosed with cancer and 75,030 died from the disease in 2019 alone, according to the AACR.
For many of the most common types of cancer, including breast, lung, prostate and colorectal, incidence and/or death rates are higher among African Americans than other racial and ethnic groups.
The AACR reports that African American men have prostate cancer incidence of 1½ times more than men of any other race or ethnicity and death rates at more than two times those of men of other races.
Several factors may contribute to these numbers, the AACR said, but it’s mostly because African American men are less likely to receive aggressive treatment after a prostate cancer diagnosis. That could be related to the culture in which many African Americans and Black people are raised.
“In some communities like the Black community, it’s sometimes frowned upon to actually say the word cancer,” Blue said. “So these cancers aren’t discussed and that often leads to someone not getting the treatment necessary or from even sharing the hereditary impact of a certain disease type.”
Nature vs. Nurture
Studying disparities like these comes down to one question, Blue said. “Is it a nature versus nurture issue?” And that question spans the cancer spectrum.
African Americans have a death rate that is at least double that for white people when it comes to multiple myeloma and stomach cancer, the AACR reports. The higher stomach cancer rate could be linked to the cancer-causing bacterium Helicobacter pylori, which is twice as common in Black people than among white people. For multiple myeloma, a blood cancer, rates may be impacted by obesity rates, which are higher among African Americans and Black people in general.
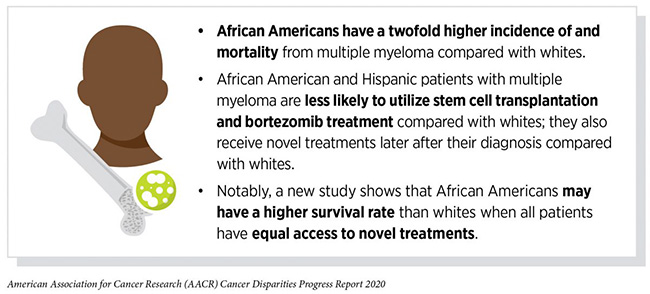
“In these blood cancers, such as multiple myeloma, lymphoma and leukemia, we see that same pattern that African Americans seem to have a worse prognosis,” Blue said. “They live a shorter lifespan compared to someone from a different ethnic background. We’re really trying to erase that and make things better for that group of people.”
Obesity rates could also be to blame for the substantial disparities in colorectal cancer incidence and death rates among Black people and African Americans. Screening rates are also skewed. The AACR presented one study estimating that 42% of the incidence rate disparity and 19% of death rate disparities were attributable to differences in colorectal screening rates.

Access — or lack of access — to cutting edge treatment is a big factor in cancer disparities in the Black community.
“Your environment and location have a big impact on your health,” said Dr. Tiffany Carson from the Health Outcomes and Behavior Program at Moffitt. “If you live in an area that is not near health care or you lack transportation to get to a doctor, your risk increases. If you’re living in an area that is not walkable or doesn’t provide access to healthy foods, your risk increases. Unfortunately, this type of living environment impacts the African American and Black communities more, which ultimately raises cancer risks.”
Breast Cancer in Black Women
Breast cancer is the most commonly diagnosed cancer among African American women, with 33,840 new cases estimated to have been diagnosed in 2019, the AACR reports. While the incidence rates are similar among Black and white women, the death rate is 39% higher for African American women.
Many factors contribute to the breast cancer death rate disparity, including African American women being more likely to be diagnosed at a later stage of disease, when treatment is less likely to be successful, and being more likely to be diagnosed with triple-negative breast cancer, which is a biologically aggressive form of breast cancer with a poor prognosis.

Dr. Kimberley Lee, a medical oncologist in the Department of Breast Oncology, notes there are large differences in the way in which Black women receive treatment for breast cancer compared to their white counterparts, likely leading to those disparities.
“We know that Black women are more likely to be undertreated or mistreated and less likely to get the drugs or surgery that they need,” said Lee, who is currently conducting a study on care delivery for Black women with breast cancer. “I am focusing on how we give them the things we know that work and focusing on that care delivery piece.”
Lung Cancer’s Impact on Black Men
Lung cancer is the leading cause of cancer death in the U.S. Historically, data have shown that Black men and women are more affected by the disease than white men and women. However, African American/white disparities in lung cancer incidence and death rates are not striking.
The AACR dissects the numbers, though, and found that when men and women are considered separately, the disparities unfold. Lung cancer incidence rates are 13% higher among African American men compared to white men and 14% lower among African American women compared with white women.
Trends are similar when considering lung cancer death rates. African American men see death rates from lung cancer at 18% higher than their white counterparts. Lung cancer death rates for African American women are 12% lower than white women.
These numbers are directly related to smoking rates in the Black community, the AACR reports. African American women smoke cigarettes at a lower rate than white women. African American men, however, smoke cigarettes at a higher rate than white men.
“What we do in our daily lifestyle impacts our overall health,” Carson said. “Our lifestyle behaviors — diet, physical activity and smoking — all have patterns that are different across racial and ethnic groups and one of the reasons for that could be cultural. It’s important to educate all communities about healthy choices if we are ever going to improve these cancer rates.”



