First CAR-T Gene Therapy for the Treatment of Cancer Gains FDA Approval
The U.S. Food and Drug Administration has approved a pioneer CAR T-cell gene therapy, leading a pack of novel treatments that promise to change the standard of care for certain aggressive blood cancers. The first-of-its-kind, Kymriah (tisagenlecleucel) will treat certain pediatric and young adult patients with a form of acute lymphoblastic leukemia (ALL). The FDA advisory panel voted unanimously to recommend approval of the treatment following a study showing a single dose of Kymriah left 83 percent of participants cancer-free after three months.
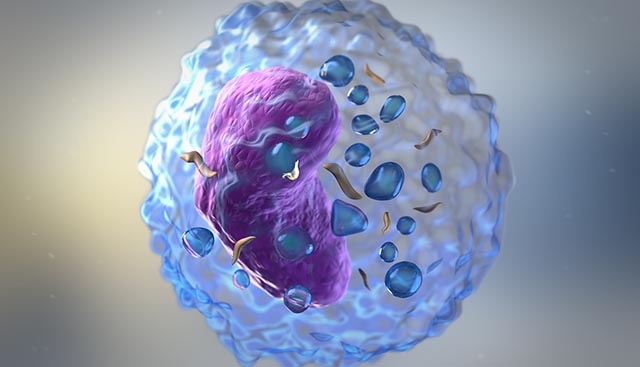
Moffitt Cancer Center is one of the few U.S. cancer centers certified to offer this therapy to patients. Each dose is custom-tailored for an individual patient. Moffitt's Fred Locke, MD explains how CAR T is used to reprogram a patient’s own cells to seek out and destroy cancer cells: "We take immune system cells from the blood of the cancer patient. These immune system cells, called T cells, normally fight against infection.
"We ship them to a central manufacturing facility where they're engineered. A gene, the CAR gene, is put in those T cells. The cells are then shipped back to the treating center where we infuse them into the vein of the cancer patient."
The patient’s genetically modified T-cells' new gene contains a specific protein (a chimeric antigen receptor or CAR) that directs the T-cells to target and kill leukemia cells that have a specific antigen (CD19) on the surface.
"Then those now CAR-T cells circulate through the body and they go seek out the cancer cells, find them and destroy them."
Like Novartis with Kymriah, Kite Pharma, soon to be acquired by Gilead Sciences, is also in active development of cell therapies for liquid and solid tumors. KTE-C19, an investigational form of autologous CAR T-cell therapy also directed against CD19, is awaiting FDA approval for aggressive B-cell lymphomas.
"This is a revolution. It's a revolution in cancer care. This is the tip of the iceberg," says Dr. Locke.
Treatment with CAR T therapies has the potential to cause severe side effects, including cytokine release syndrome (CRS), which is a systemic response to the activation and proliferation of CAR T-cells causing high fever and flu-like symptoms, and for some, neurological events. Both CRS and neurological events can be life-threatening.
Thus, in tandem with Kymriah, the FDA jointly expanded the approval of Actemra (tocilizumab) to treat CAR T-cell-induced CRS. In clinical trials in patients treated with CAR-T cells, 69 percent of patients had complete resolution of CRS within two weeks following one or two doses of Actemra.
Because of the risk of CRS and neurological events, the FDA is requiring that hospitals and their associated clinics that dispense Kymriah be specially certified. At Moffitt Cancer Center, staff involved in the prescribing, dispensing, or administering of Kymriah are required to be trained to recognize and manage CRS and neurological events.
About Dr. Locke
Dr. Frederick Locke is a medical oncologist and translational researcher in Moffitt's Department of Blood and Marrow Transplant and Cellular Immunotherapy. He leads the Immune Cell Therapy (ICE-T) initiative at Moffitt, an integrated cross-departmental translational team. Dr. Locke is a clinical research leader in the field of Chimeric Antigen Receptor (CAR) T cell therapy, acting as a national P.I. for several pivotal trials of anti-CD19 CARs for lymphoma. In addition, Dr. Locke is translating findings from his laboratory into new cellular immunotherapies such as the Moffitt-created whole protein survivin tumor vaccine for multiple myeloma. More...
