Georgios Papanikolaou: Inventor of the Pap Smear Test
The American Cancer Society estimates that more than 14,000 Americans will be diagnosed with cervical cancer in 2021, and more than 4,000 will die from the disease. It was once one of the leading causes of cancer death for American women. Thanks to Dr. Georgios Papanikolaou, the cervical cancer death rate dropped significantly following his discovery of what we know as the Pap test, or Pap smear, in 1941.
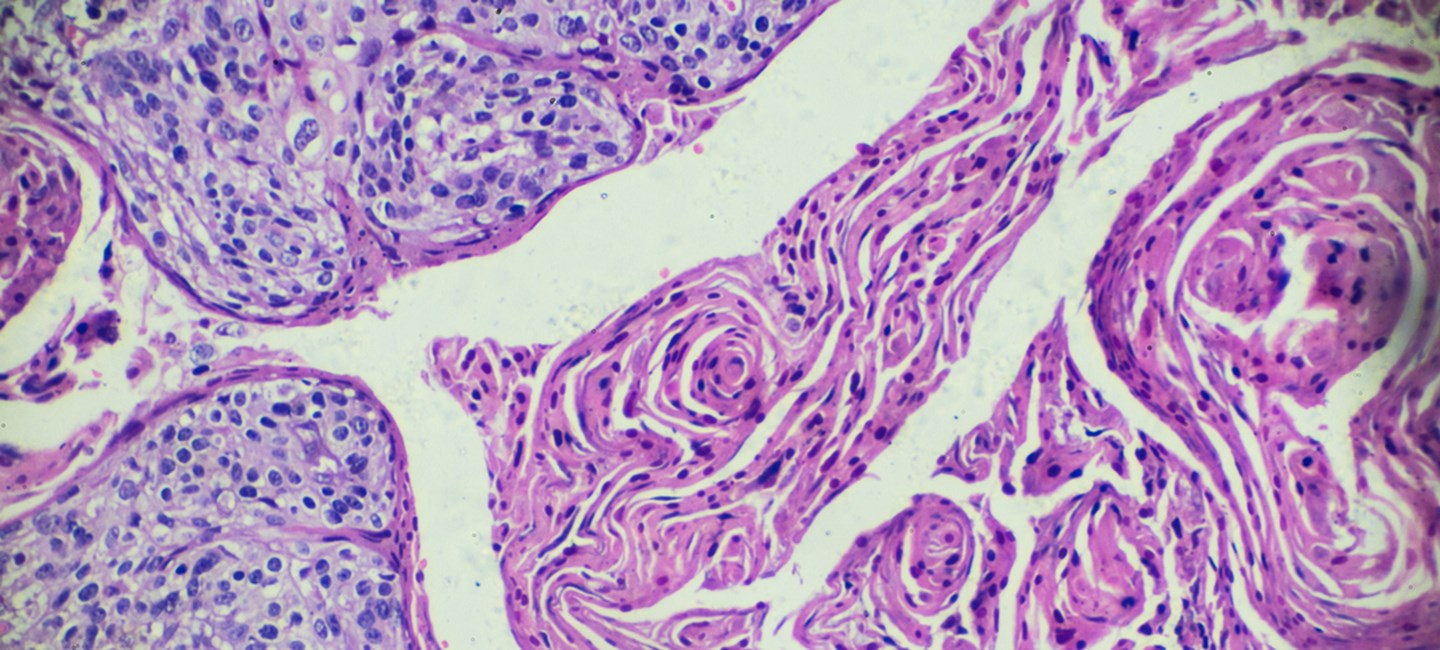
Born in Greece, Papanikolaou began his research career studying the reproductive cycles of guinea pigs. After moving to the United States, he changed his focus to human physiology and began working with Dr. Herbert Traut, a gynecologist at Cornell University. The two published Diagnosis of Uterine Cancer by the Vaginal Pap Smear in 1943. This test detailed how normal and abnormal vaginal and cervical cells could be viewed under a microscope and how they should be classified. The Pap smear quickly became the standard in cervical cancer screening, and it is still the primary screening tool for cervical cancer today.
“Among one of the great success stories in cancer was the development of a simple swab of the cervix and a smear on a slide to detect changes associated with precancer of the cervix,” said Dr. Robert Wenham, chair and research director for Gynecologic Oncology at Moffitt Cancer Center. “It led to a dramatic decline in a terrible cancer that affects some of the youngest women with gynecologic cancer.”

How was cervical cancer diagnosed before the Pap smear? According to Dr. Barbara Centeno, director of Moffitt’s Cytology Laboratory, the disease often wasn’t discovered until it was too late.
“Women were dying of cervical cancer that went undetected until it was in the late stages,” said Centeno. “Patients previously would have to present symptoms like bleeding, painful intercourse or vaginal secretions which at that point would really be advanced stage cancer.
Infection caused by the human papillomavirus (HPV) is one of the biggest risk factors for cervical cancer. The American Cancer Society recommends routine HPV vaccination between ages nine and 12. Children and young adults ages 13 through 26 who haven't been vaccinated, or who haven't gotten all their doses, should get the vaccine as soon as possible.
Cervical cancer screening with an HPV test is recommended every 5 years for everyone with a cervix from age 25 to 65. If HPV testing alone is not available, people can get screened with an HPV/Pap co-test every 5 years or a Pap test every 3 years.
“In more recent times, the understanding of HPV and its role in the cancer has led to even better detection with HPV testing,” said Wenham. “The vaccines available may stop it before it ever needs to be detected and help make this a rare or never cancer. In fact, the HPV test and vaccination will likely eliminate the Pap smear altogether someday, but we owe much to the smear test and the women’s lives it has saved.”