Fewer Transfusions for Patients with MDS?
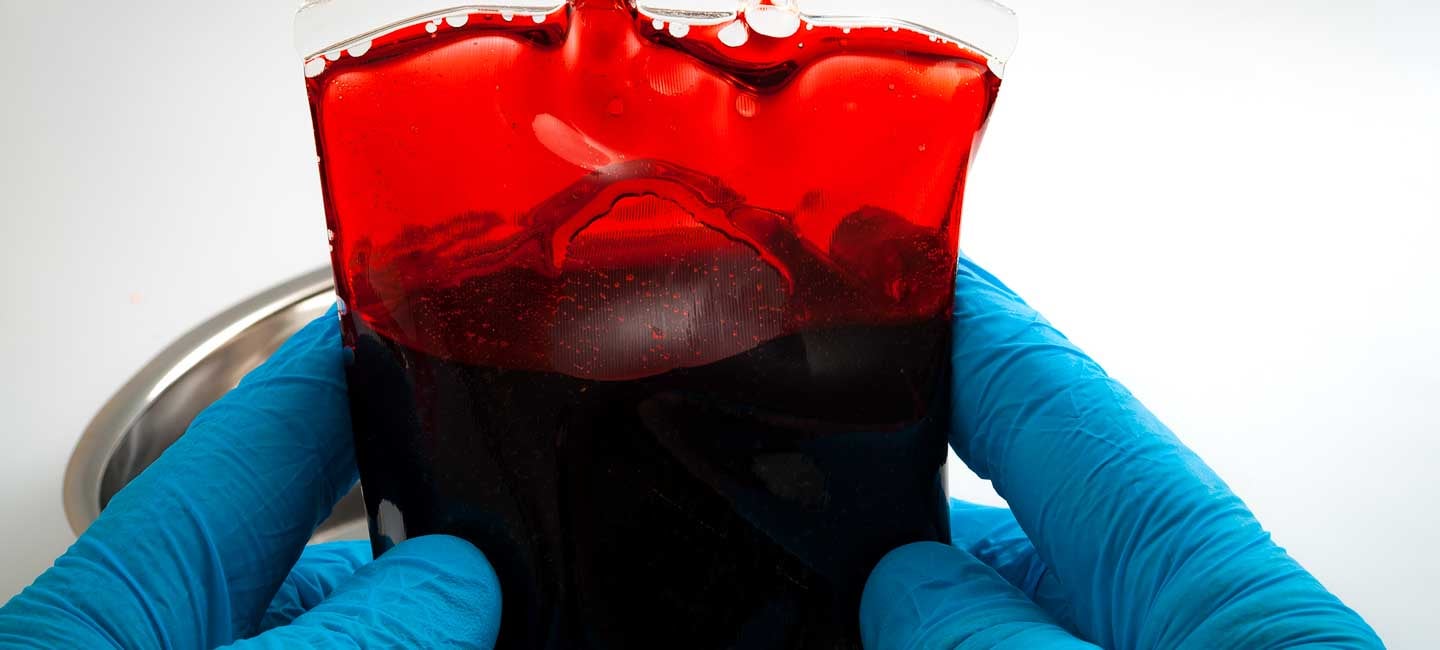
For patients with myelodysplastic syndromes (MDS), blood transfusions can be a necessary part of life. But results of a recently reported clinical trial show a new drug helped more than half of patients with a lower-risk form of MDS to avoid or profoundly reduce transfusions. If ultimately approved for use by the U.S. Food and Drug Administration, it would become the first new drug for this patient population in more than a decade.
The findings were presented by Dr. Alan List, President and CEO of Moffitt Cancer Center, in a plenary session of the annual meeting of the American Society of Hematology (ASH) in early December. Dr. List, an internationally known scientist, practicing hematologist and senior co-author of the study, noted the new drug could be a “game-changer” for transfusion-dependent, lower-risk MDS patients.
Dr. Alan List, President and CEO of Moffitt Cancer Center, speaking at the annual meeting of the American Society of Hematology (ASH) in December 2018.
Each year, some 10,000 Americans are diagnosed with MDS, a family of cancers of the bone marrow that interfere with a person’s ability to manufacture healthy blood cells. Those with aggressive forms of MDS may develop bleeding, infections or leukemia. Even with lower-risk MDS, patients usually battle anemia. Many harbor a genetic mutation (SF3B1) linked to slower production of mature, healthy red blood cells. Available anemia drugs like erythropoietin only help about half of these patients, leaving the rest dependent on lifelong, frequent blood transfusions that are costly, inconvenient and can lead to other health issues.
Previous studies of a targeted drug called luspatercept had shown promise of increasing red blood cell levels in this patient population. It works by blocking certain proteins that slow down the body’s red blood cell production. The MEDALIST clinical trial was designed to evaluate the safety and effectiveness of luspatercept for reducing transfusion dependence in lower- to intermediate-risk MDS patients. The double-blind, placebo-controlled trial enrolled 229 adult patients who did not respond to available anemia drugs and required transfusions every month or two. Ninety percent of the participants had an SF3B1 mutation. All were randomly assigned to receive either the drug or a placebo via injection every three weeks for at least six months.
Results of the phase 3 MEDALIST clinical trial showed more than a third (38 percent) of patients receiving luspatercept went at least eight weeks without the need for a transfusion, with approximately 40 percent of responders remaining transfusion free at one year. Among the placebo group, only 13 percent reached this primary endpoint. Overall, more than half (53 percent) of patients receiving luspatercept saw either a significant drop in the number of transfusions needed or an increase in their hemoglobin levels without transfusion. Only 12 percent of the placebo group achieved these measures. Reported side effects of the drug were minimal.
“Severe anemia resulting in red blood cell transfusion dependence is a significant challenge for patients with low- and intermediate-risk MDS. Those who become resistant or refractory to currently available treatments have limited alternatives,” Dr. List stated in a press release from the drug’s manufacturers Celgene Corporation and Acceleron Pharma. “The findings from MEDALIST are very exciting as they support the hypothesis that targeting red blood cell precursor maturation could help to address patients’ anemia and allow them to achieve transfusion independence.”
News of the MEDALIST study has received international attention from medical and scientific journals. During the ASH conference, Dr. List was interviewed by reporters from STAT, BioWorld, Hematology News, ASCO POST, MedPage Today, eCancer, ASH Clinical News, MD Magazine, VJ HemOnc, Congress Report and BioPharma Dive.
Dr. List is internationally recognized for his many contributions in the development of novel, more effective treatment strategies for MDS and acute myeloid leukemia. His pioneering work led to the development of lenalidomide (Revlimid®) from the laboratory to clinical trials, which went on to receive fast-track designation from the U.S. Food and Drug Administration and approval for the treatment of patients with MDS and multiple myeloma.
The next step for luspatercept is for its developers, Celgene Corporation and Acceleron Pharma, to file for FDA approval, a move that is expected sometime in 2019.