‘A Clinical Trial Saved My Life’
When Larry Thomason saw the number of doctors coming into the room to discuss his case with him in March 2016, he braced himself for some bad news.
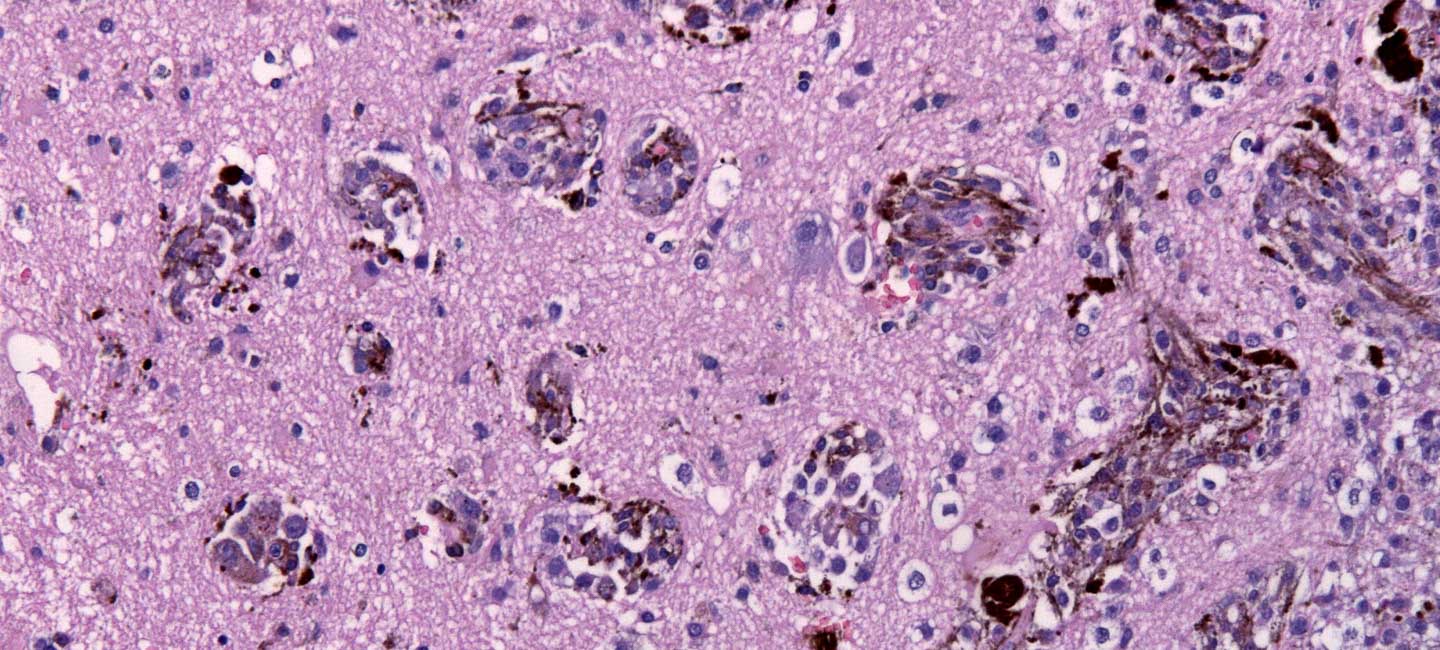
Thomason’s instinct was right. The melanoma surgically removed nearly two years before had returned and traveled throughout his body, including his brain. Several metastatic nets in his brain caused hemorrhaging and swelling that could potentially impact his motor skills and speech.

Larry Thomason with wife Nancy.
“They told me they didn’t even know how I was functioning,” Thomason said. “Then they told me the prognosis – I had six to 10 months left and most of that would be spent in hospice. There was no known FDA-approved treatment option that wouldn’t hinder the quality of life I had left.”
But fortunately for Thomason, Peter Forsyth, M.D., chair of the Department of Neuro-Oncology at Moffitt Cancer Center, had one more suggestion for the retired 3M vice president. A new form of immunotherapy was in a clinical trial that combined nivolumab (Opdivo) and ipilimumab (Yervoy). The trial offered at least some promise.
“It was a glimmer of hope that we could grab on to,” Thomason said.
Thomason was one of the earliest patients on the trial, Forsyth said, and it was hard to predict exactly how he would fare.
“This was – and is – a new tool in our arsenal to battle these types of tumors,” Forsyth said. “This treatment turns on your T cells to attack the tumors. It’s like making little soldiers angry. It’s good when they are angry because they want to attack things; but sometimes they fire too much and that can result in friendly fire on healthy organs. So there are known complications.”
Forsyth encouraged Thomason and his wife, Nancy, to relocate to Tampa from Florida’s Panhandle, at least for a few months so he could monitor the treatments.
“To deal with any side effects, I wanted him close by,” Forsyth said. “That way we could manage them.”
Thomason followed Forsyth’s suggestion and soon found himself at Moffitt receiving regular infusions of the drugs through an IV. Five weeks later, doctors had their first major update.
“Two of the five largest tumors were just gone,” Thomason said. “The remaining tumors had reduced by more than half. I couldn’t believe it.”
And neither could Forsyth, who admits he was amazed by the treatment’s effectiveness.
“The results were better than expected, just amazing,” Forsyth said. “He is not only alive, but he’s living. And it’s all because of that clinical trial.”
Thomason continued the treatment every three weeks and repeatedly saw positive results. Other than a rash at one point, side effects were minimal for him and he said he was never incapacitated, despite the initial swelling in his brain.
Today he is considered cancer-free and is living an active life. He walks eight miles every day and travels quite a bit with his wife. But every three months he gets screened to keep the cancer in check.
“Larry is able to enjoy life. He is healthy and in remission, and I hope that goes on for many years,” Forsyth said. “We are fortunate that we have a multidisciplinary practice here at Moffitt and that I’m able to work with experts in melanoma and other areas. That, along with the treatment, likely saved his life.”
Thomason is thankful for the second chance at life he received at Moffitt and said that while it wasn’t easy, putting his trust in his doctors was the best decision he could have made.
“A clinical trial saved my life,” Thomason said. “I had to accept that my team of doctors knew what was best for me and it worked.”