Immunotherapy for Head & Neck Cancer
Head and neck cancer is a broad term that refers to several different malignancies that can develop in the mouth, salivary glands, throat or nose. Most are squamous cell carcinomas that form in the flat-cell layer (epithelium) that lines the mouth, throat and nose. While the vast majority of head and neck cancers are caused by tobacco use, some cases are also linked to the Epstein-Barr virus or the human papilloma virus (HPV).
Treatment options for head & neck cancer
When detected early, many head and neck cancers are very treatable. Some options include chemotherapy, radiation therapy, surgery and immunotherapy. The optimal approach can vary based on a number of individual factors, such as the exact location of the tumor, the stage of the cancer and the patient’s general health.
Due to the location of many head and neck tumors, treatment can sometimes affect a patient’s ability to eat, swallow or breathe. Immunotherapy is a promising treatment option that can help some patients avoid these complications. In essence, immunotherapy involves boosting the body’s own immune system to help it fight off the cancer.
While there are many types of immunotherapies, only one type is currently approved by the U.S. Food and Drug Administration (FDA) for the treatment of advanced head and neck cancers: immune checkpoint inhibitors. Immune checkpoint inhibitors for advanced head and neck cancers are only standardly used for patients whose cancers cannot be cured by chemotherapy, radiation, or surgery. Adoptive cellular therapies are a different type of immunotherapy that represents a promising new strategy to treating advanced head/neck cancers. These will both be discussed below.
“Every day that I was at Moffitt, I always came home enriched. You get to the point where you don’t want to leave because you just feel like it’s home.”
Ellen, neck and thyroid cancer survivor
Request an appointment
Immune checkpoint inhibitors
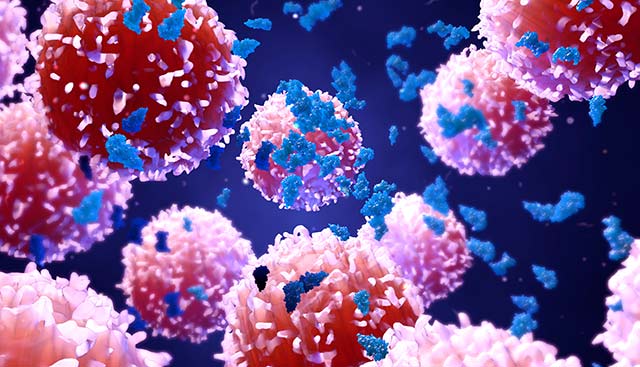
The immune system plays a vital role in inhibiting the development of head and neck tumors. Through a complex series of steps known collectively as the immune response, the immune system helps keep the body healthy by targeting and attacking bacteria, viruses, cancer and other harmful invaders that can cause disease.
Through extensive research studies, scientists have identified various “checkpoint” proteins that regulate the immune response and help prevent the immune system from targeting healthy tissues. While these checkpoints are effective for that purpose, they are sometimes exploited by cancerous cells. As a result, the cancer is able to evade detection and destruction by the body’s immune system and continues to grow.
Immune checkpoint inhibitors are drugs that work by releasing the natural “brakes” on the immune system, helping it to recognize and attack cancerous tumors that are masquerading as checkpoint targets. For instance, PD-1 is a protein found in certain immune cells (T cells). Normally, PD-1 functions as an “off switch” that prevents the T cells from attacking healthy cells. More specifically, the T cells are switched off whenever PD-1 attaches to PD-L1, a protein found in many normal cells. However, because PD-L1 is also found in some cancerous cells, those cells are able to avoid detection and attack.
Immunotherapy drugs known as monoclonal antibodies are designed to target either PD-1 or PD-L1, which can prevent those proteins from binding and boost the immune response against cancer.
Adoptive cellular therapies
Adoptive cellular therapy is a type of immunotherapy that involves taking a sample of a patient’s own immune cells (T cells or tumor-infiltrating lymphocytes), modifying those cells and then reintroducing the altered cells to the patient’s body, where they can seek out and destroy cancerous cells. One example of adoptive cellular therapy is CAR T-cell therapy, in which a patient’s T cells are fortified with chimeric antigen receptors (CARs) to bolster their cancer-fighting activity.
Three cell-based immunotherapies that are currently being evaluated in head and neck cancer clinical trials are:
- HPV-related antigens – These drugs target proteins expressed by HPV-infected cancer cells.
- EBV-related antigens – These drugs target the foreign viral proteins expressed by EBV-infected cancer cells.
- MAGE antigens – These drugs reactivate the genes that produce MAGE proteins, which are normally turned off in adult cells, to help the immune system identify cancerous cells as invaders.
The challenging aim of immunotherapy for head and neck cancer is to selectively direct the cellular destruction mechanisms of the immune system toward cancerous cells while leaving healthy cells unharmed. To achieve this highly selective targeting, it is necessary to identify the specific protein sequences that are found exclusively in tumor cells and recognized by T cells and tumor-infiltrating lymphocytes.
Groundbreaking immunotherapy initiatives at Moffitt Cancer Center
The scientists and clinicians at Moffitt Cancer Center are making great strides in advancing the treatment of many types of head and neck cancer, and we continue to explore and develop novel cellular immunotherapies and other treatment options. If you’d like to learn more, you can request an appointment with an oncologist in our Head and Neck Cancer Program. Call 1-888-663-3488 or complete a new patient registration form online. We do not require referrals.
