Moffitt Cancer Center Uses AI to Develop More Personalized Cancer Treatment Strategies
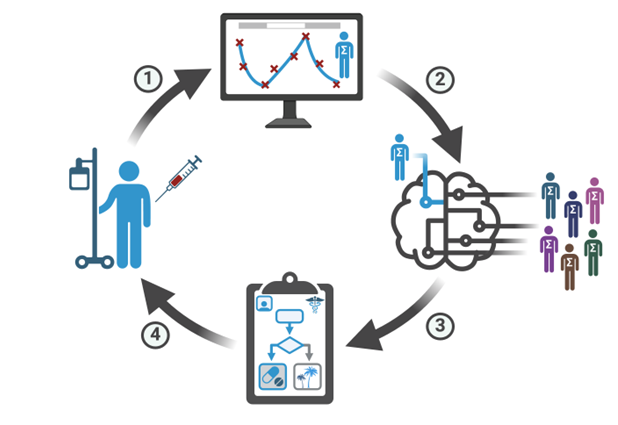
TAMPA, Fla. — Conventional treatment strategies, which focus on maximal cell killing, frequently fail against metastatic cancers due to the emergence of drug resistance. Adaptive therapy strategies, which dynamically adjust treatment to suppress the growth of treatment-resistant populations, have emerged as a promising alternative. However, the lack of truly personalized approaches limits their efficacy. In a study published online ahead of print in Cancer Research, a team of Moffitt Cancer Center researchers introduce a novel framework that leverages deep reinforcement learning to tailor adaptive treatment schedules, potentially doubling the time to progression compared to current standard-of-care protocols.
Lead investigator Sandy Anderson, Ph.D., co-director of the Center of Excellence for Evolutionary Therapy at Moffitt, along with long term collaborator Philip Maini, Ph.D., director of the Wolfson Centre for Mathematical Biology at the University of Oxford, say this study’s significance lies in its ability to generate interpretable and personalized adaptive treatment schedules. “By integrating evolutionary principles and mathematical models into adaptive therapy decision-making, our research opens new avenues for translating innovative treatment approaches into clinical practice,” Anderson said.
First author Kit Gallagher, a University of Oxford student, applied deep reinforcement learning, a type of artificial intelligence, to create adaptive therapy schedules for prostate cancer. He used a virtual patient model to train the deep reinforcement learning system. It uses a mathematical model developed at Moffitt by Maxi Strobl, who is now postdoc at Cleveland Clinic, to account for tumor dynamics allowing for adaptability to individual patients. The results showed that the new personalized approach significantly outperformed standard-of-care treatments and existing adaptive therapy approaches.
“Interpretability has long been a significant hurdle to integrating machine learning approaches into clinical practice. While these frameworks are a black-box, and we can’t understand how they derive treatment recommendations, we can’t be confident applying these in the clinic,” Gallagher said.
The researchers are planning further studies to refine this method and explore its application to other forms of cancer.
“Model driven personalized medicine is the future of cancer treatment,” Anderson said. “By harnessing the power of deep reinforcement learning, we can optimize treatment strategies for each patient, leading to better outcomes and improved quality of life.”
This work is supported by the National Cancer Institute (U01CA232382; U54CA274507).
About Moffitt Cancer Center
Moffitt is dedicated to one lifesaving mission: to contribute to the prevention and cure of cancer. The Tampa-based facility is one of only 57 National Cancer Institute-designated Comprehensive Cancer Centers, a distinction that recognizes Moffitt’s scientific excellence, multidisciplinary research, and robust training and education. Moffitt’s expert nursing staff is recognized by the American Nurses Credentialing Center with Magnet® status, its highest distinction. For more information, call 1-888-MOFFITT (1-888-663-3488), visit MOFFITT.org, and follow the momentum on Facebook, Twitter, Instagram and YouTube.
###

