Advancements in Non-Muscle Invasive Bladder Cancer Treatment
Bladder cancer, ranked as the tenth most prevalent cancer worldwide, continues to challenge healthcare providers and researchers. Amidst the complexities of managing this disease, the shortage of Bacillus Calmette-Guérin (BCG), a cornerstone in non-muscle invasive bladder cancer (NMIBC) treatment, has magnified the unmet need for innovative approaches and bladder-preserving therapies. At Moffitt Cancer Center, we're committed to providing our patients with treatment options, including access to novel approaches that give hope to patients with NMIBC.
Understanding NMIBC
The majority of newly diagnosed bladder cancer cases are NMIBC, making up 75% of all bladder cancers. Characterized by cancer cells confined to the inner lining of the bladder, NMIBC poses a significant clinical challenge due to its high recurrence rate and risk of progression to muscle-invasive cancer. Stratifying patients into risk groups based on various factors such as tumor stage, grade, and prior recurrences guides oncologists in making treatment decisions, which traditionally include Transurethral Resection of Bladder Tumor (TURBT), a surgical procedure to remove visible tumors from the bladder lining, followed by intravesical anti-cancer therapies, such as BCG (live attenuated bacteria to stimulate an immune response against cancer cells) or chemotherapy. For decades, this has been the standard of care.
Other standard treatment approaches, which aim to prevent recurrence and progression while preserving bladder function, include:
- Intravesical Chemotherapy - For patients who cannot tolerate BCG or aren’t appropriate candidates, intravesical chemotherapy, such as mitomycin C. or gemcitabine, may be considered. In addition, we are participating in a clinical trial investigating the efficacy of dual chemotherapy gemcitabine and docetaxel, to provide equivalent efficacy for NMIBC.
- Maintenance Therapy: Maintenance BCG and chemotherapy may be recommended to reduce the risk of recurrence. Maintenance schedules vary by patient.
- Cystoscopy and Surveillance: Regular cystoscopies are performed to monitor for recurrence. If new tumors are detected, additional treatments may be initiated.
Navigating the BCG Shortage
BCG is used as an intravesical immunotherapy for NMIBC, but it is also used as the tuberculosis vaccine. Both utilize the same bacteria strain of Mycobacterium bovis, but BCG for NMIBC is weakened before use to reduce bodily harm. Standard intravesical BCG is successful in 60-70% of patients with NMIBC, and high-grade patients should receive full-strength BCG for best results.
However, because BCG is also widely used to protect populations against tuberculosis, and because of several other factors, there’s a shortage of this critical immunotherapy.
Other components impacting the availability of BCG include:
- Manufacturing challenges - Cultivating the live bacteria needed is time-consuming and complex. Issues with production facilities or regulatory compliance all contribute to limited supply.
- Supply chain issues - Disruptions in the supply chain, such as transportation issues, raw material shortages, and other geopolitical factors, can impact access.
The North American shortage of BCG significantly impacts NMIBC management and care and has prompted the exploration of alternative strategies to manage the disease effectively.
Embracing Innovation: Novel Alternative Treatment Approaches
The FDA has approved many alternative treatment methods for NMIBC, and several others are being investigated in clinical efficacy trials.
Immunotherapy options can be highly effective at reducing recurrence rates and improving patients' quality of life and survival rates. Immune checkpoint inhibitors (ICI), including Pembrolizumab, have shown promising results in the treatment of high-risk BCG-unresponsive NMIBC and were recently FDA-approved. However, it’s toxic, expensive, and may not be effective compared to radical cystectomy (RC) or salvage intravesical chemo. It’s currently the classic second-line treatment for NMIBC, but other immunotherapies, such as intravesical immunotherapy, are also an option. One type that Moffitt uses includes nadofaragene firadenovec, a gene therapy utilizing a modified virus to enhance the immune response within the bladder by exploiting cytokine mechanisms.
In addition to alternative treatments, other strategies include reducing BCG dose, delaying treatment, closely monitoring the patient (especially for low-risk patients), or enrolling eligible patients in clinical trials.
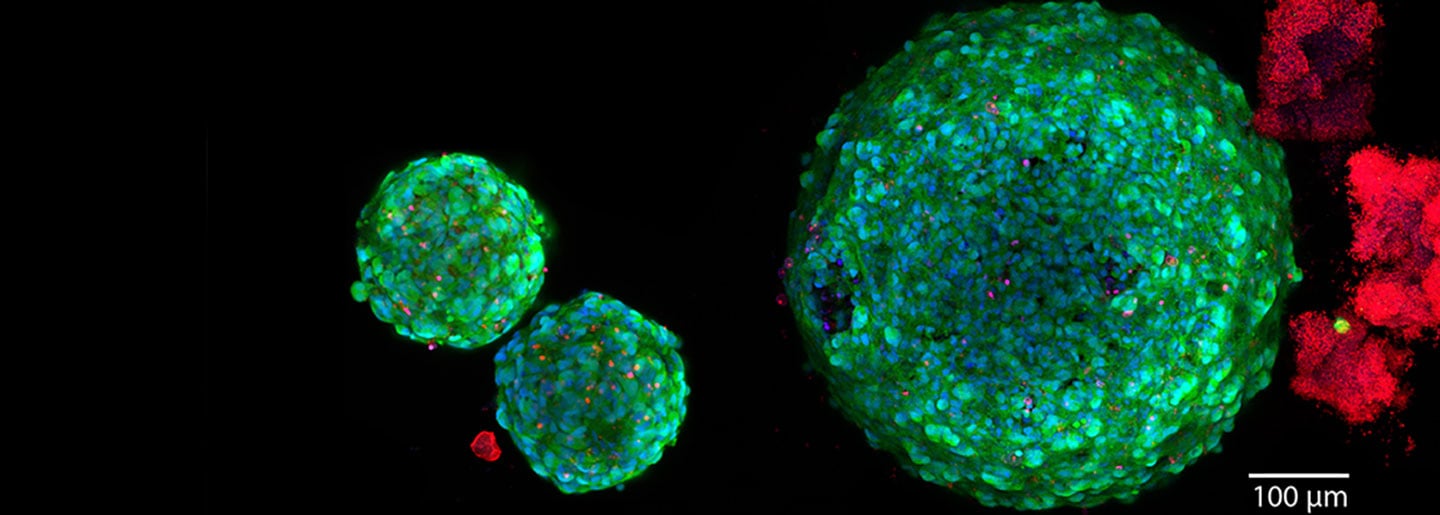
Clinical trials are crucial to advancing the quality of care for bladder cancer patients, forming the cornerstone for future NMIBC treatment and better patient outcomes. Dr. Roger Li, an internationally recognized expert in novel drug development, has led several global registrational trials to bring new and efficacious bladder-sparing options to patients with bladder cancer. He is the principal investigator for Phase 1B Single-Arm Study of CG0070 After Transurethral Resection in Patients With Intermediate Risk NMIBC and the Phase 1 Study of Erdafitinib Intravesical Delivery System (TAR-210) in Participants with Non-Muscle-Invasive or Muscle-Invasive Bladder Cancer and Selected FGFR Mutations or Fusions. Both trials are currently open for enrollment. Another Phase 3, randomized controlled trial (MoonRISe-1) will be activated soon at Moffitt, testing the efficacy of TAR-210 vs. conventional intravesical chemotherapy in patients with intermediate-risk NMIBC. These trials offer patients access to leading-edge treatments and lay the foundation for future advancements in NMIBC care.
Expanding Options for NMIBC Care
From exploring promising immunotherapies to utilizing clinical trials, Moffitt is dedicated to creating new treatment paths for NMIBC patients who don’t respond to BCG and considering the global shortage of BCG. With several treatment options available and multispecialty teams who work collaboratively to optimize care plans, Moffitt patients have the best chances of beating cancer.
We encourage providers to refer patients with NMIBC to Moffitt to explore their treatment options.
If you’d like to refer a NMIBC patient to explore treatment options at Moffitt , complete our online form or contact a physician liaison for assistance. As part of our efforts to shorten referral times as much as possible, online referrals are typically responded to within 24 - 48 hours.
2024 Cell Coast Conference
October 25-27, 2024 - Tampa, FL
Join us for an exclusive summit featuring updates and breakthroughs in research and treatment in the cell therapies space from global thought leaders.
Event Details