Basal Cell Carcinoma Information
Basal cell carcinoma is a common type of nonmelanoma skin cancer that makes up the majority of cancer diagnoses in the United States. An estimated 3.6 million cases are diagnosed in the U.S. every year, and numbers are on the rise. Comparatively, 1.8 million cases of squamous cell carcinoma—the other primary form of nonmelanoma skin cancer—are diagnosed annually.
What is basal cell carcinoma?
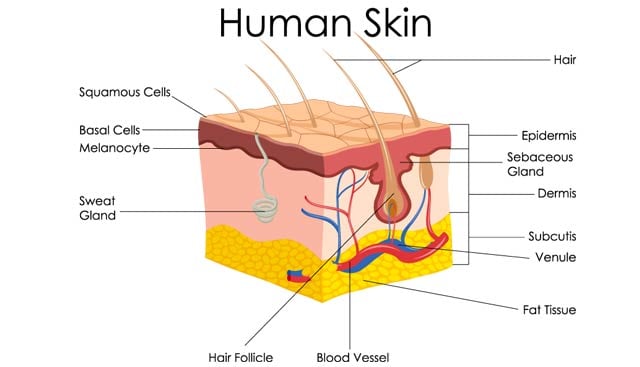
Basal cell carcinoma is a skin cancer that begins in the basal cells, which are responsible for producing new skin cells as old cells die off. Unlike other types of skin cancer, basal cell carcinoma rarely spreads (metastasizes) beyond the area in which it originally develops.
Basal cell carcinoma vs. squamous cell carcinoma
Basal cell and squamous cell carcinomas are the two most common types of skin cancer. Together, along with Merkel cell carcinoma, they are collectively known as nonmelanoma skin cancer. Squamous cell carcinoma rarely spreads to other areas of the body, although it does so more often than basal cell skin cancer. As its name suggests, squamous cell carcinoma develops in the skin’s flat, scale-like squamous cells that line the outer layer of the epidermis.
Basal cell carcinoma vs. melanoma
Melanoma is the most dangerous form of skin cancer. Unlike basal cell carcinoma, melanoma often spreads to distant organs if left untreated. It originates in the skin’s pigment-producing cells (melanocytes) and presents as a new or unusual mole that can change shape, size or color over time.

Basal cell carcinoma causes and prevention
Most experts agree that long-term exposure to ultraviolet (UV) radiation from sunlight is responsible for basal cell carcinoma, which is why the best way to prevent this skin cancer is to limit your time in the sun and regularly apply a broad-spectrum sunscreen of SPF 15 or higher when you’re outside—even on cloudy days. Here are a few other steps you can take:
- Wear protective clothing, sunglasses and a broad-brimmed hat when outside.
- Stay in the shade, or schedule outdoor activities in the early morning (before 10 a.m.) and evening (after 4 p.m.).
- Avoid using tanning beds and sunlamps.
It’s also recommended to see a dermatologist annually for a professional skin exam and routinely perform self-checks for changes in your skin, particularly on your face, scalp and other areas of your body that are often left uncovered.
Some people are more susceptible to sun damage than others and have greater risk of basal cell carcinoma. For example, individuals who have fair skin, freckles, blue or green eyes or red or blonde hair are considered more likely to develop skin cancer. Other risk factors for basal cell carcinoma include:
- Being older
- Being male
- Having a history of burns or inflammatory skin diseases
- Exposure to radiation and substances like arsenic, coal tar and paraffin
What are the symptoms of basal cell carcinoma?
Basal cell carcinoma typically occurs on areas of the body that are frequently exposed to the sun, such as the face, scalp, ears, neck, back and shoulders, although it can develop anywhere on the body. While the specific warning signs of this cancer can vary, it usually presents as one of the following skin lesions:
- A shiny bump that may appear pink, red, white or clear (in darker skin tones, the bump may be black or brown and look like a mole)
- An open sore that may ooze, crust or bleed and does not heal after several weeks
- A pink growth with rolled edges and a central depression
- A red patch of skin that may itch, crust or cause pain
- A taut, shiny area of white or yellow skin with irregular borders that may resemble scar tissue
- An unusual pigmented growth
Not all skin abnormalities indicate cancer. Only a physician can diagnose or rule out basal cell carcinoma, so it’s important to promptly consult with a medical professional if any changes in skin occur.
Basal cell carcinoma types
There are multiple types of basal cell carcinoma, including:
- Nodular basal cell skin cancer – The most common subtype, this cancer typically presents as a round, shiny bump.
- Superficial basal cell skin cancer – This subtype may appear as a scaley plaque with defined borders.
- Pigmented basal cell skin cancer – A very rare nonmelanoma skin cancer that may resemble melanoma.
- Invasive (sclerosing) basal cell skin cancer – An uncommon and complex cancer that can appear as pale scar tissue in its initial stages.
Basal cell carcinoma survival rate and prognosis
 The overall prognosis for basal cell carcinoma is excellent, especially when it is diagnosed in an early stage. Today’s treatment approaches for this skin cancer offer an 85% to 95% recurrence-free cure rate. In rare cases, basal cell carcinoma can be disfiguring or life-threatening if it is left untreated.
The overall prognosis for basal cell carcinoma is excellent, especially when it is diagnosed in an early stage. Today’s treatment approaches for this skin cancer offer an 85% to 95% recurrence-free cure rate. In rare cases, basal cell carcinoma can be disfiguring or life-threatening if it is left untreated.
Squamous cell and basal cell carcinoma deaths are not officially reported, but it’s estimated that roughly 2,000 people die of these nonmelanoma skin cancers every year in the U.S., with squamous cell cancer comprising the majority of deaths. Skin cancers are more dangerous in older populations and people with compromised immune systems.
Diagnosing basal cell carcinoma
To confirm a diagnosis of basal cell carcinoma, a physician will perform a biopsy and send the sample to a pathologist for further evaluation in a lab. One of several biopsies may be recommended depending on the size and shape of the skin lesion:
- A shave biopsy – Top layers of the skin are gently scraped off with a sharp blade.
- A punch biopsy – A small, round instrument is used to “punch” and remove a deeper section of the skin.
- An excisional biopsy – Surgical techniques are used to remove the entire lesion, along with a small margin of surrounding healthy skin.
Moffitt Cancer Center’s approach to basal cell carcinoma treatment
At Moffitt Cancer Center, we take an innovative, multispecialty approach to treating basal cell carcinoma. In our Cutaneous Oncology Program, an experienced team of oncologists (all of whom focus exclusively on the treatment of skin cancer) will review each patient’s case to determine which therapies would be most suitable. After considering the cellular makeup of the cancer, the patient’s ability to tolerate certain treatments and a number of other unique factors, our tumor board may recommend:
- Surgery – Most basal cell carcinomas can be surgically managed through a traditional excision, but our experienced skin cancer surgeons can also perform more complex operations (e.g. a lymph node resection or a graft reconstruction) in cases of advanced basal cell carcinoma.
- Radiation therapy – Moffitt’s radiation oncologists can formulate a treatment plan that delivers the maximum safe dose of ionizing radiation to a cancerous lesion, while minimizing exposure to nearby healthy skin.
- Immunotherapy – These therapies target various molecules in the body (such as the protein interleukin-2) to induce an immune response to the basal cell carcinoma.
- Chemotherapy – Topical chemotherapy can be used to treat precancerous lesions, while systemic chemotherapy drugs may be administered to address basal cell carcinomas that have reached the lymphatic system and spread to distant organs.
Several other treatments, such as adoptive cell therapy and intralesional therapy, are also available through our robust clinical trial program. As a National Cancer Institute-designated Comprehensive Cancer Center, we are at the forefront of groundbreaking research that benefits not only our patients but every individual who has been diagnosed with basal cell carcinoma. Plus, these trials allow us to provide our patients with access to the widest possible range of therapies in one convenient location.
To learn more about basal cell carcinoma treatment at Moffitt Cancer Center, call 1-888-663-3488 or complete a new patient registration form. As Florida’s top cancer hospital, we’re expanding access to world-class care by connecting patients with cancer experts rapidly.
