
Minimally Invasive Surgery Advancements for Spinal Tumor Surgery
Dr. James Liu is a neurosurgeon who specializes in the surgical and radiosurgical treatment of brain and spinal tumors. He’s an expert in using minimally invasive techniques for the treatment of spinal tumors to provide restoration of spinal stability and improve quality of life with minimal disruption of systemic or radiation therapies. Here are five questions with Dr. Liu on minimally invasive techniques for spinal tumor surgery.
What is the Moffitt Minimally Invasive Spine Oncology (M-MISO) program?
The Minimally Invasive Spine Oncology (MISO) program at Moffitt Cancer Center is patient-centered with a focus on the use of minimal access techniques for the treatment of metastatic spine disease from solid or hematological malignancies. The goals of MISO surgery include rapid pain relief, preservation of neurologic function, and restoration of spinal stability.
What are some of the latest MIS surgery techniques?
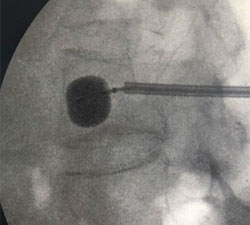 Cement augmentation (Kyphoplasty) and radiofrequency ablation (RFA) - Cement augmentation is used for cancer-related painful compression fractures from metastatic disease or multiple myeloma. It is performed as an outpatient procedure. Pain relief is often immediately observed following the procedure.
Cement augmentation (Kyphoplasty) and radiofrequency ablation (RFA) - Cement augmentation is used for cancer-related painful compression fractures from metastatic disease or multiple myeloma. It is performed as an outpatient procedure. Pain relief is often immediately observed following the procedure.
Radiofrequency ablation (RFA) - RFA uses thermal ablation to treat tumors within the spinal column and is often used in conjunction with kyphoplasty to provide additional pain control.
 Percutaneous pedicle screw fixation with cement augmentation - When metastatic disease involves the posterior aspect of the spinal column beyond just the vertebral body, percutaneous pedicle screw fixation can be used to provide spinal stability through small incisions for each pedicle screw, without the need for a large midline incision and disruption of a significant amount of paraspinal musculature.
Percutaneous pedicle screw fixation with cement augmentation - When metastatic disease involves the posterior aspect of the spinal column beyond just the vertebral body, percutaneous pedicle screw fixation can be used to provide spinal stability through small incisions for each pedicle screw, without the need for a large midline incision and disruption of a significant amount of paraspinal musculature.
What is the difference between cement augmentation (Kyphoplasty) vs. percutaneous pedicle screw fixation?
Although both these procedures can be considered ‘minimally invasive’ interventions, they have very different indications. When disease involves the posterior aspect of the spinal column beyond just the vertebral body, cement augmentation alone is not enough to provide adequate stability to result in meaningful pain relief. In these cases, when there is no neural compression that requires open decompression, percutaneous pedicle screw fixation can be performed to provide spinal stability.
Patients with metastatic disease often have diffusely poor bone quality which can result in failure of spinal instrumentation. To avoid the need for long fusion constructs, we use fenestrated screws when placing percutaneous pedicle screws. This provides a cement augmentation at the tips of the screws to increase the strength of the construct, thus allowing effective spinal stabilization with short-segment constructs.
Who are the patients most likely to benefit from MIS procedures?
Minimally invasive surgery can potentially help any type of spinal tumor patients, especially patients with metastatic disease from solid or hematological malignancies who do not need open decompression of neural structures. Determining the most appropriate type of MIS intervention would allow for the least invasive procedure with the most effective relief. Additionally, MIS techniques are recommended for any type of spine tumor patient who would benefit from spinal stabilization with minimal delay or disruption of systemic treatments.
What are some of the signs and symptoms that require follow-up with a specialist?
Pain
- Midline back pain with a known malignancy
- Pain that gets worse at night or when lying flat
- Mechanical back pain – pain worse with movement and relieved with rest
Neurological symptoms
- Weakness in unilateral or bilateral extremities
- Numbness, tingling in the extremities
- Pain radiating in the extremities that get worse with movement
Radiographic findings
- Evidence of multi-level bone marrow changes or a lytic lesion in the vertebral bodies
- Fractures of vertebral bodies on X-rays, CT, or MRI
- Evidence of epidural disease with spinal canal stenosis, foraminal stenosis, or neural compression
- Loss of natural curvature of the spine, e.g., kyphotic deformity secondary to collapsed vertebrae
At Moffitt, we consider it a privilege to partner with referring providers to care for our shared patients. After surgery, we can arrange for the patient to receive treatment within his or her local community if desired. We also provide second opinions consult on a full range of complex neurologic cancers and conditions in a single, convenient location.
To learn more about Moffitt’s MISO program or to discuss a specific patient, please contact your physician liaison to set up a virtual meeting with Dr. Liu. Or, if you’d like to refer a patient to Moffitt, complete our online form or contact a physician liaison for assistance. As part of our efforts to shorten referral times as much as possible, online referrals are typically responded to within 24 - 48 hours.
