Personalizing Breast Cancer Radiation Treatment
By Kim Polacek
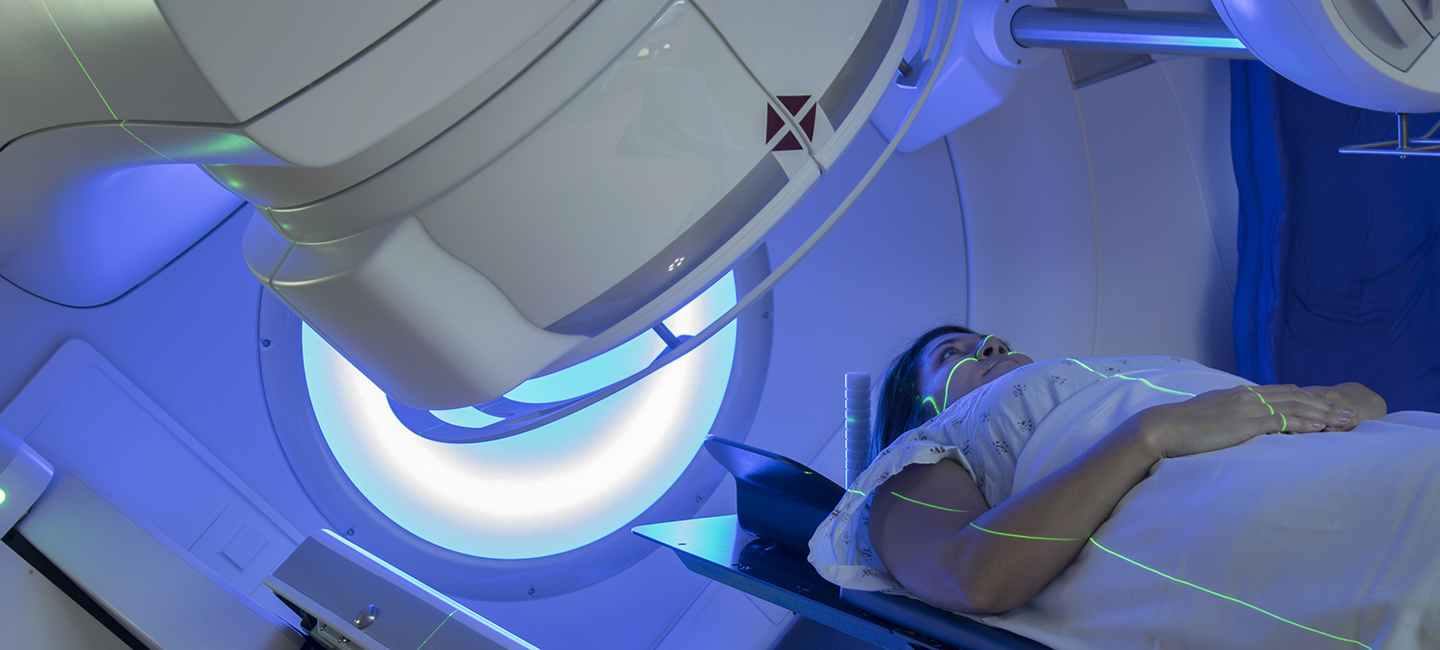
Precision therapy is the future of oncology. This approach personalizes a patient’s treatment based on their genetics and cancer type. There are numerous drugs now available that target a particular tumor type and genetic mutation. However, this same personalized strategy has not translated to radiation therapy, which follows a one-size-fits-all approach for most patients.
Moffitt Cancer Center is hoping to change that mindset. Our physician-scientists have developed a genomically based model that can optimize and personalize a radiation dose to match an individual patient’s needs.
Radiation therapy is part of the standard treatment approach for breast cancer, but the dose administered to most patients is largely the same. While there are clinical studies being conducted to determine the benefits and risks of omitting radiation treatment in certain patients with breast cancer who are at a low risk of local disease recurrence, a genomic approach to personalize radiotherapy dose has not yet been undertaken.

Dr. Javier Torres-Roca, a radiation oncologist at Moffitt, has been working on personalized radiation therapy. Several years ago, he developed and validated a radiation sensitivity index to predict the radiation sensitivity of tumors based on the patterns of 10 genes. Now, he is advancing the index one step further to more accurately determine the appropriate radiation dose for individual patients. Combining the radiation sensitivity index with a model that is used to determine the effect of radiation dose on tumor and normal tissues, he created a new radiation dose determining method called genomically adjusted radiation dose, or GARD.
“GARD is the first opportunity for a genomically driven personalized approach in radiation oncology, and is a research priority for the field,” explained Torres-Roca. “Our research has found that GARD values are lower for those tumors that are resistant to radiation and higher for those tumors that are sensitive to radiation treatment.”
Torres-Roca and his colleagues in Moffitt’s Department of Radiation Oncology are planning several clinical trials in breast and head and neck cancers where patients’ radiation therapy dose will be selected based on the GARD model. These trials will be the first to test a genomic approach to personalized radiation therapy dose in the field of radiation oncology. He hopes through continued study and its implementation into practice that the model will benefit patients by allowing a personalized approach to radiation treatment and will minimize the risks of additional radiation exposure.