New CAR T Therapy Tested for Multiple Myeloma
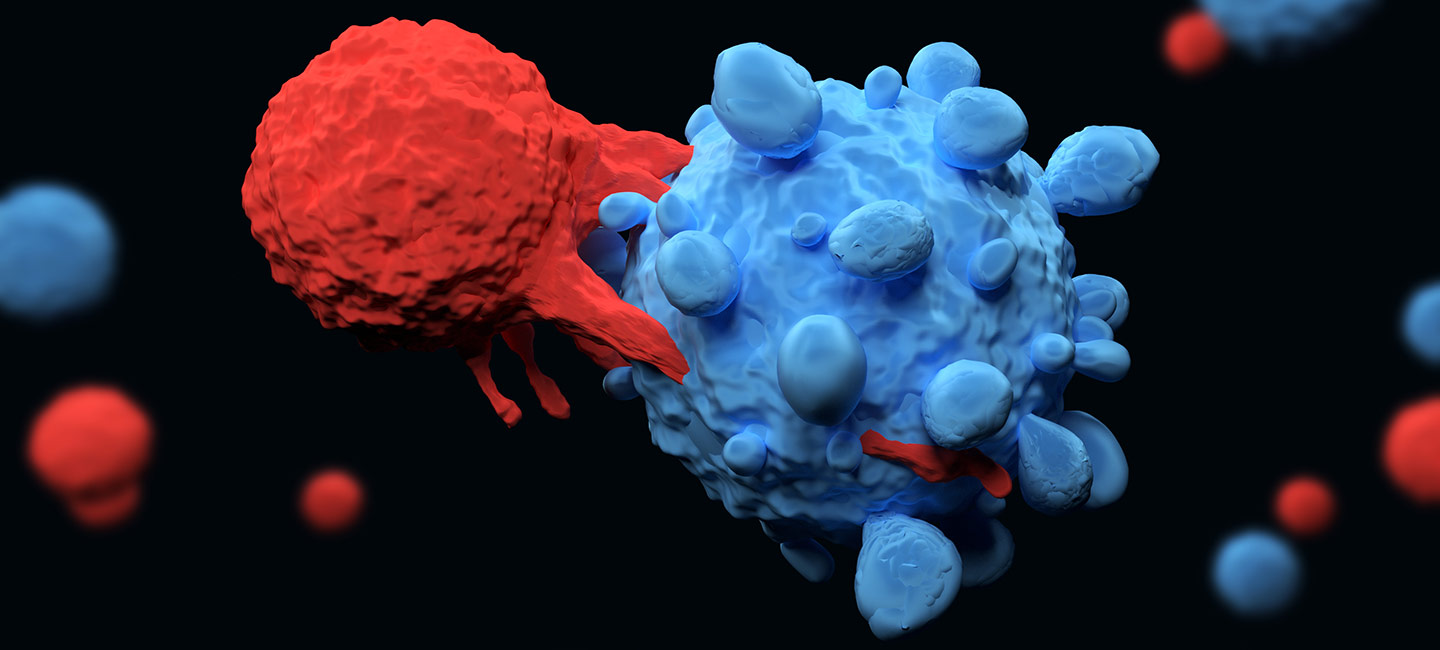
Immunotherapy, specifically chimeric antigen receptor T cell therapy or CAR T, has been a hot topic in the blood cancer field. Currently, there are several CAR T therapies approved for the treatment of leukemia and lymphoma. Now, researchers are working to develop new types of CAR T and cellular immunotherapies that can treat additional blood cancers and solid tumors.
One area where they are making progress is multiple myeloma. This type of cancer arises from plasma cells. The exact cause is not known and there is no cure. There are several treatment options that can provide durable responses for patients. However, as patients have disease progression, the disease becomes resistant to therapy, and this group of patients with relapsed/refractory multiple myeloma have very few treatment options.

Dr. Melissa Alsina, Head of Multiple Myeloma Program, Blood and Marrow Transplant & Cellular Immunotherapy Department
“Even with all the current treatment options, with time, it is challenging to treat patients with relapsed/refractory multiple myeloma because with subsequent therapies the disease becomes resistant, the rates of complete remission decrease and the duration of response shortens,” said Dr. Melissa Alsina, head of the Multiple Myeloma Program of the Blood and Marrow Transplant and Cellular Immunotherapy Department at Moffitt Cancer Center.
Alsina, along with other investigators, is working with Bluebird Bio, Inc. to investigate a new CAR T product for patients with relapsed/refractory multiple myeloma. The therapy targets B-cell maturation antigen (BCMA), a protein found on the surface of malignant plasma cells. Like other CAR T therapies, a patient’s immune cells are removed using a process called apheresis. The immune cells are then re-engineered in the lab to attach the anti-BCMA receptor to each cell. This receptor will act as a GPS to allow the immune cells, once infused back into the patient, to seek out and destroy the cancerous cells.
“This product (bb21217), uses the same CAR molecule as bb2121, an anti BCMA CAR T developed by Bristol Myers Squibb, but the cells are cultured with a PI3 kinase inhibitor to enrich for T cells displaying a memory-like phenotype. The idea is that this enrichment will make the CAR T cells persist and work against the myeloma for longer, potentially resulting in more durable responses,” said Alsina.
Updated results from the phase 1 trial, which Alsina presented at the American Society of Hematology Annual Meeting, show patients are responding well to the therapy.
“The treatment is not without side effects, with the most common toxicities being low blood counts, cytokine release syndrome and infections, which are all common toxicities for CAR T therapies, but very manageable,” said Alsina.
Of the 59 patients who received the investigational therapy and could be evaluated for response at the time of the analysis, 68% responded to the therapy, with 29% having a complete response, meaning no detectable signs of disease. Also, and most encouraging, investigators saw persistence of the CAR T cells in some patients for up to 24 months after therapy, and a median duration of response of 17 months, consistent with the hypothesis that enriching drug product for memory like T cells may result in improved durability of response. This is early data with a median follow-up of only six months, but Alsina says the team is hoping that these results will be confirmed as the data matures.