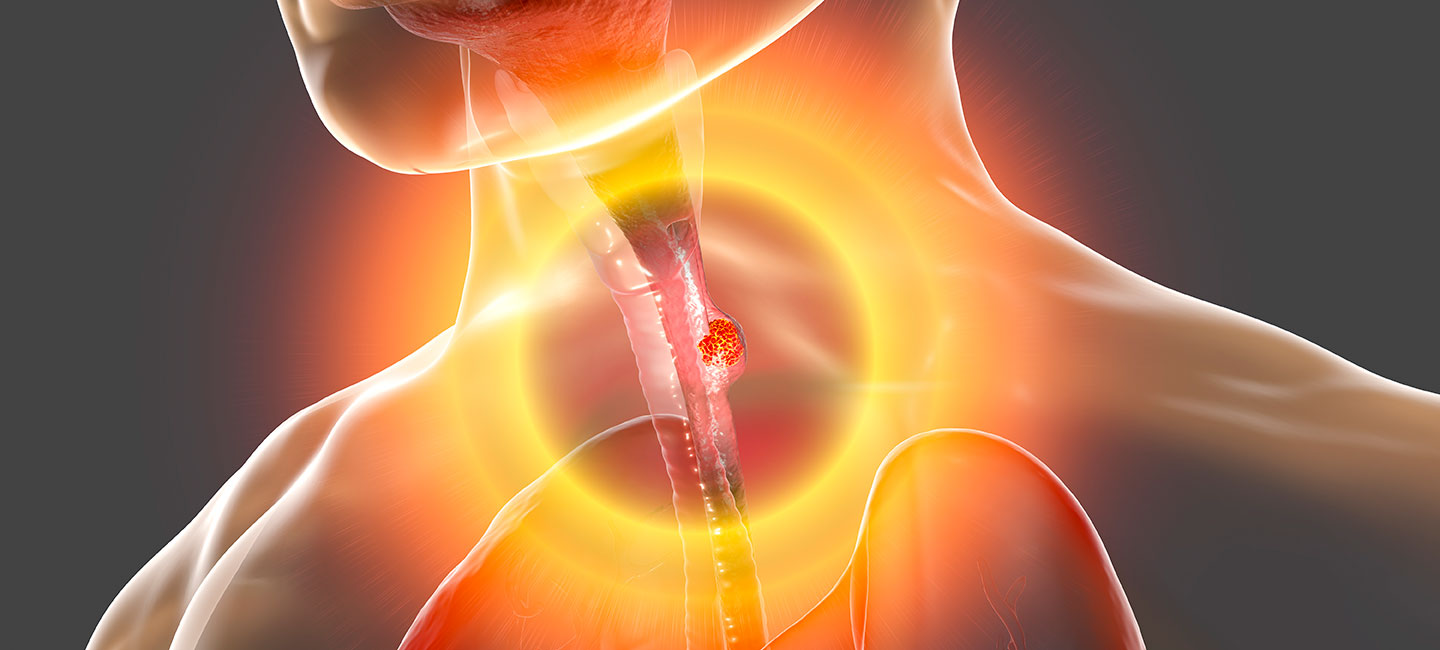
Immunotherapy Makes Big Strides in Esophageal Cancer
Esophageal cancer has one of the lowest survival rates of all cancers, and patients who don’t respond to initial treatment or remain at high risk for recurrence have few options. However, for the first time ever, immunotherapy is offering new hope.
There are two types of esophageal cancer: squamous cell carcinoma and adenocarcinoma. Squamous cell carcinoma is usually caused by smoking, drinking or past radiation to the chest, while risk factors for adenocarcinoma — the more common type — are obesity, acid reflux and gastroesophageal reflux disease. While there are more treatment options for adenocarcinoma, both types have similar survival outcomes.
After diagnosis of either type of esophageal cancer, staging the cancer is very important because it dictates treatment. For early stage cancer, the tumor can usually be removed. Cancer that is locally advanced — stage 2 and 3 — is treated with chemoradiation followed by surgery. However, up to 75% of patients do not have a complete response to treatment, and until now there were no recommendations for additional treatment.
Results from a phase 3 clinical trial published in the New England Journal of Medicine show an immunotherapy drug called nivolumab prolonged disease-free survival in patients who failed first line treatment.

Dr. Rutika Mehta, medical oncologist, Gastrointestinal Oncology
“As of 2020, the standard of care was chemoradiation and surgery, but there was no additional treatment,” said Dr. Rutika Mehta, a medical oncologist in the Gastrointestinal Oncology Program at Moffitt Cancer Center. “This is a paradigm shift because this is something really new in this space. It is something new we can do for patients who have residual disease at the time of surgery.”
Patients who received nivolumab (Opdivo®) on the trial had an average disease-free survival of 22.4 months, compared with 11 months among patients who received a placebo.
“When we make advances, we make them one step at a time, so from a patient’s perspective I can see that the benefit might seem small, but for a space where we had nothing to offer before this is a huge step forward,” said Mehta.
The trial wasn’t the only big step forward. In March, the U.S. Food and Drug Administration approved pembrolizumab (Keytruda®) in conjunction with chemotherapy to treat metastatic esophageal cancer. The study that led to the approval found the treatment regimen improved overall survival, reducing the risk of death by 27%. The impressive benefit was mostly found in patients with squamous cell carcinoma who express a high level of PD-L1, a protein that helps keep immune cells from attacking nonharmful cells in the body.
While pembrolizumab plus chemotherapy has proved to be a successful first line treatment for squamous cell carcinoma patients, Mehta says adenocarcinoma patients would need to be carefully selected for the treatment.
Just a few weeks ago, Bristol Myers Squibb announced promising results from another ongoing trial that is evaluating treatment with nivolumab plus chemotherapy or nivolumab plus another immunotherapy drug called ipilimumab (Yervoy®) in patients with metastatic esophageal squamous cell carcinoma. The pharmaceutical company says both treatment regimens demonstrated a statistically significant and clinically meaningful benefit in patients whose tumors express PD-L1 and in the all-randomized patient population. Moffitt is one of the sites that participated in the trial.