Bridging Therapy Not Recommended for All CAR T Patients
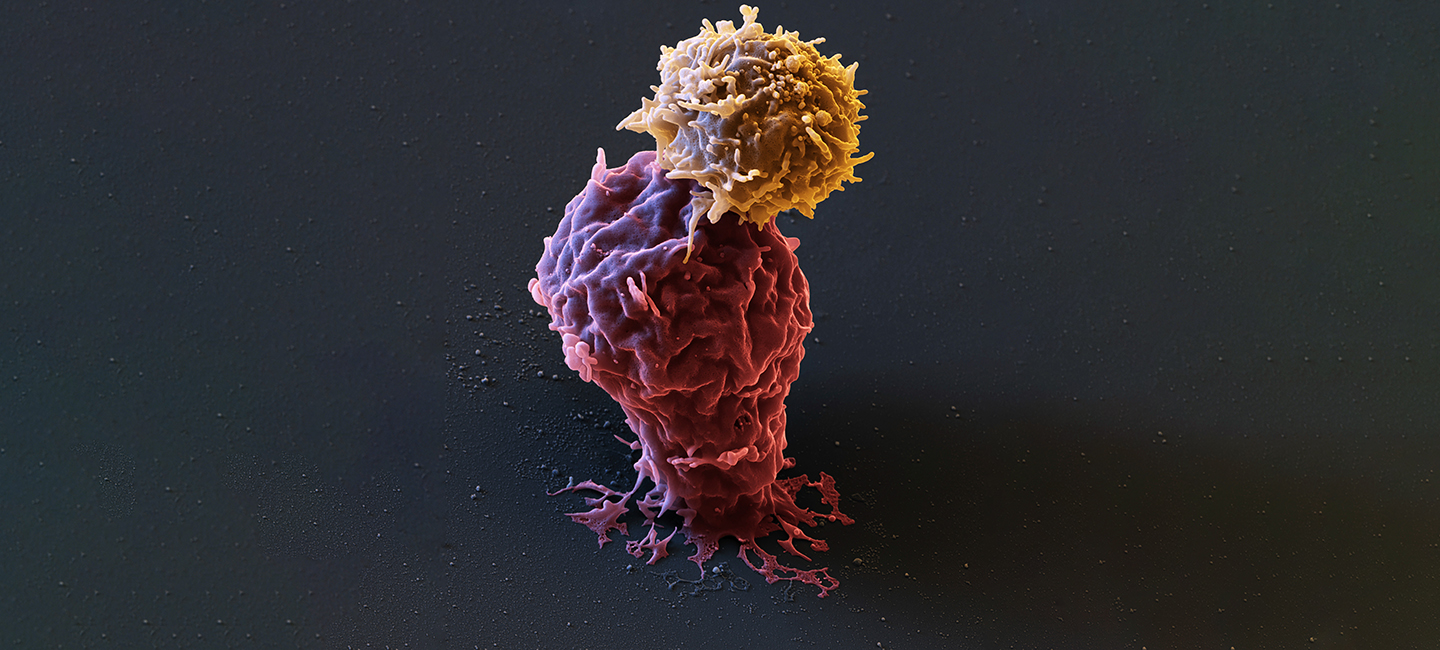
Chimeric Antigen Receptor T-cell therapy, or CAR T for short, can provide good outcomes for patients with diffuse large B cell lymphoma (DLBCL) who have failed other therapies and/or have relapsed. More than 40% of patients who received Yecarta®, one of the two FDA-approved CAR T products for DLBCL, have seen durable responses. But for patients who have relapsed or are in declining health, there are some downsides to the therapy.

Dr. Michael Jain, assistant member, Blood and Marrow Transplant and Cellular Immunotherapy Department at Moffitt Cancer Center
“Once we’ve collected the patient’s T cells and shipped them to the production facility, it can take up to three weeks to receive the re-engineered CAR T cells back from the manufacturer,” said Dr. Michael Jain, assistant member of Moffitt’s Blood and Marrow Transplant and Cellular Immunotherapy Department. “Often a patient may need some type of intervention during that window of time to prevent further decline. There can also be severe toxicities once the therapy has been administered.”
Moffitt Cancer Center is one of 17 institutions that make up the U.S. CAR T Lymphoma Consortium. Physicians from this group of cancer treatment centers pool data and outcomes from their CAR T patient populations to ask questions that can help optimize care and administration of the therapy. To date, they have information on nearly 300 patients who received Yescarta after the therapy was approved and made available commercially.
Jain and his collaborators looked at the consortium data to determine if administering a bridging therapy – radiation, chemotherapy, steroids or targeted therapy – could help patients in declining health who were waiting for their CAR T treatment to be scheduled. He presented the findings Dec. 7 at the 61st American Society of Hematology Annual Meeting in Orlando, Fla.
Of the 298 patients included in the data set, 158 received some type of bridging therapy. Conversely, patients who did not require bridging therapy had excellent outcomes, with 80% of patients still alive one year after CAR T treatment.
“We found that overall response was worse for patients who received bridging therapy prior to CAR T-cell therapy,” said Jain. “This does not mean bridging therapy should be abandoned for this group of patients; however, doctors do need to be careful when selecting if and what bridging therapy a patient should receive before their CAR T infusion."